How Oral Bacteria Affect Your Health
A combination of genetic and environmental risk factors contribute to heart disease, which is responsible for about a third of all deaths worldwide. A buildup of plaque in the arteries that supply blood to the heart causes coronary artery disease, the most common type of heart disease, and can also block blood vessels, causing heart attacks. Previous studies have already linked certain infections to an increased risk of plaque formation. According to a new study published in eLife, becoming infected with a special bacterium that causes gum disease and bad breath can increase your risk of heart disease.
Certain Strains of Bacteria Increase the Risk of a Cardiovascular Event
Although tremendous progress has been made in understanding how coronary artery disease develops, understanding of how infection, inflammation and genetic risk factors contribute is still incomplete. Hodel and colleagues analyzed genetic information, health data and blood samples from a subset of 3,459 people who participated in the CoLaus|PsyCoLaus study – a population-based cohort in Switzerland. Of the 3,459 participants, approximately 6% experienced a heart attack or other deleterious cardiovascular events during the 12-year follow-up period. The team tested the participants’ blood samples for the presence of antibodies against 15 different viruses, six bacteria and one parasite. After adjusting the results for known cardiovascular risk factors, the authors found that antibodies to Fusobacterium nucleatum (F. nucleatum), a sign of past or current infection by the bacterium, were associated with a slightly increased risk of a cardiovascular event.
According to the researchers, F. nucleatum could contribute to cardiovascular risk through increased systemic inflammation due to the presence of bacteria in the mouth or through direct colonization of artery walls or plaque lining the artery walls. The authors also confirmed that individuals with high genetic risk scores for coronary artery disease have an increased risk of cardiovascular events, as previous studies have shown. According to the authors, if future studies confirm the link between F. nucleatum and heart disease, this could lead to new approaches to identify individuals at risk or prevent cardiovascular events.
Oral Bacteria and Hypertension
Bacterial strains in the mouth can also lead to high blood pressure, according to research. Hypertension is an important risk factor for cardiovascular disease and stroke. In a study of more than 1,200 women in the US with an average age of 63, 10 types of oral bacteria were associated with a higher risk of developing hypertension in postmenopausal women, while five bacterial strains were associated with a lower risk of hypertension. The observational study cannot prove cause and effect, but the results highlight possible ways to improve the prevention of hypertension through targeted oral hygiene.
Hypertension is typically defined by two measurements: systolic blood pressure (the top number measures the pressure when the heart is beating) of 130 mm Hg or greater and diastolic blood pressure (the bottom number indicates the pressure between heartbeats) of 80 mm Hg or greater .
Researchers analyzed data from 1,215 postmenopausal women at the Buffalo Osteoporosis and Periodontal Disease Study in Buffalo, New York. Upon enrolling in the study, researchers recorded blood pressure and collected oral plaque below the gum line, where some bacteria keep gums and tooth structures healthy and others cause gum and periodontal disease. They also recorded medication intake and medical and lifestyle histories to determine if there was a link between oral bacteria and high blood pressure in older women.
At study entry, approximately 35% of study participants had normal blood pressure: readings below 120/80 mm Hg, without taking any blood pressure medication. Almost 24% of the participants had elevated blood pressure: readings above 120/80 mm Hg without taking any medication. Approximately 40% of the participants were classified as patients with predominant treated hypertension: diagnosed and medicated hypertension. The researchers identified 245 unique strains of bacteria in the plaque samples. Almost a third of the women who did not have hypertension at baseline or were not treated for hypertension were diagnosed with hypertension during the follow-up period, which averaged 10 years.
10 Types of Bacteria Increase the Risk of High Blood Pressure
The analysis found that 10 types of bacteria were associated with a 10-16% higher risk of developing hypertension, five other types of bacteria were associated with a 9-18% lower risk of developing hypertension. The potential associations for the same 15 bacteria subgroups at risk of hypertension were analyzed comparing women under 65 years of age with women over 65 years of age; smoker versus non-smoker; those with normal versus elevated blood pressure at baseline and other comparisons. The results remained consistent between the compared groups.
The results are particularly relevant for postmenopausal women, as the prevalence of hypertension is higher in older women than in older men. Because of the study’s observational approach, cause and effect cannot be inferred, limiting the researchers’ ability to determine with certainty that only some bacteria are associated with a lower risk of hypertension, while others are associated with a higher risk.
Oral Bacteria Can also Affect the Joints
The culprit behind a failed hip or knee replacement could be found in the mouth. DNA testing of bacteria from the fluid that lubricates hip and knee joints revealed bacteria with the same DNA as plaque from patients with gum disease who need joint replacements. This study is one of many from the Case Western Reserve University School of Dental Medicine that have linked oral bacteria to health problems when they leave the mouth and enter the blood.
The researchers hypothesize that this could be the reason why aseptic loosening or prosthetic wear of the artificial joints fails within 10 years when no infection appears to be present. It has long been suspected that these bacteria cause problems in arthritis sufferers, but scientific evidence has been lacking.
Researchers recruited and studied 36 patients being treated for osteoarthritis (joint wear and tear) and rheumatoid arthritis (an autoimmune disease) at the University Hospital’s Case Medical Center. These study participants had both natural and artificial joints. The researchers took samples of their synovial fluid, which is similar to oil that keeps a door from squeaking. These patients also had evidence of periodontitis or gum disease and underwent examinations that removed plaque for the study.
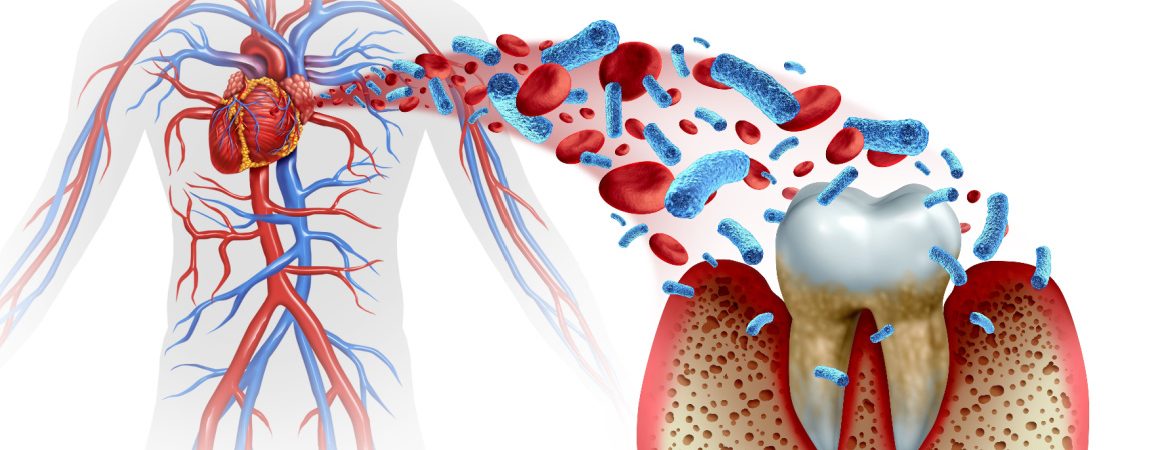
Inflammation is Triggered in the Bloodstream
Plaque buildup from bacteria associated with gum disease breaks down the walls of the pockets around teeth. The inflammatory process of the bacteria acts like a gate that allows the bacteria to enter the bloodstream. Once in the blood, the oral bacteria have triggered inflammation in remote locations where the bacteria have been linked to heart, kidney and cancer diseases, as well as premature birth and fetal death.
Because these bacteria cannot be found with routine laboratory tests, the detection of bacteria in plaque and fluid was done using a process called polymerase chain reaction and DNA sequencing of specific genes (16S-23S rRNA). This is a sophisticated DNA tracking process.
Five of the 36 patients (14%) showed direct DNA links between the bacteria in the fluid and plaque from the mouth. The patient breakdown was: one from a rheumatoid arthritis (RA) patient with a failed natural joint and one RA patient with a failed replacement joint; two osteoarthritis (OA) patients with failed artificial joints and one OA patient with a failed natural joint. Further studies are needed to investigate the precise impact of oral health on the joints.