Fertilichron Product Research
Fertilichron Product Research
Fertilichron® Male and Fertilichron® Female are breakthrough formulas that provide potent,
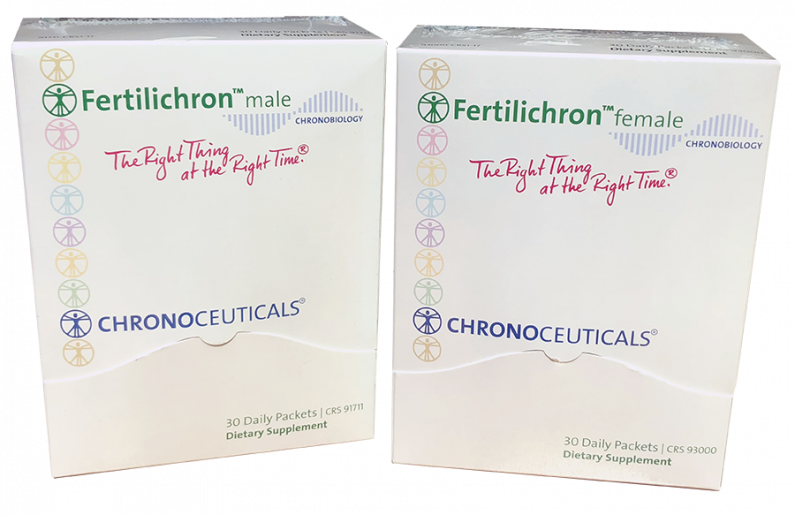
scientifically-validated phytonutrients, vitamins and essential minerals specifically chosen for their ability to support optimal reproductive health and fertility.
Provides a blend of potent medicinal plants and nutrients that naturally supports healthy male fertility and reproductive health, while also supporting healthy testosterone levels, libido and libido-related performance.
Provides the vitamins, minerals and nutrients needed for healthy female fertility, and supports optimal female reproductive health, while supporting the female body in preparation for pregnancy.
Chronobiology: The Science Behind Our Products
Chronobiology is the study of the biological rhythms and cyclic processes that make up your body’s ‘internal clock’, and how they relate to the overall functioning of the body. According to chronobiology, the internal clock regulates most bodily processes. Thus, there is an optimal time of day for proper nutrition to fully benefit each organ and biological process that takes place in the body. Due to the body’s natural rhythms, the success or failure of therapeutic measures (like supplements) may be affected by these rhythms and determine proper effectiveness.
Because so many of our bodily processes are time-dependent, theoretically, there is an optimal time of day for taking certain nutrients and plant medicines during which the benefits should be greatest.
Many different factors can affect female and male reproductive health and fertility, and certain nutrients can play an important role for men and women who wish to become pregnant, because they can help support healthy hormonal balance and a healthy reproductive system in general. Both Fertilichron Male and Fertilichron Female are formulated based on the science of Chronobiology to provide key combinations of essential nutrients and substances to help create a healthy base for reproduction.
Fertilichron Ingredient Studies & Research
Fertilichron male Research:
Systemic review of antioxidant types and doses in male infertility: Benefits on semen parameters, advanced sperm function, assisted reproduction and live-birth rate
Article: in Arab Journal of Urology 16(1) · January 2018 with 86 Reads
DOI: 10.1016/j.aju.2017.11.013
Abstract Objective: To explore the current evidence concerning the effect of oral antioxidant supplementation on various male fertility outcomes, as antioxidants are widely available compounds that are commonly used for the treatment of male infertility. Materials and methods PubMed, Medline and Cochrane electronic databases were searched according to a modified Preferred Reporting Items for Systemic Reviews and Meta-Analyses (PRISMA) guidelines looking for studies investigating the effect of antioxidant therapy on infertile men. The studies were explored looking for antioxidants: (i) types and doses; (ii) mechanism of action and rationale for use; and (iii) effect on the different outcome measures reported. Results In all, 26 studies reported a significant positive effect of antioxidant therapy on basic semen parameters, advanced sperm function, outcomes of assisted reproductive therapy, and live-birth rate. Vitamin E, vitamin C, carnitines, N-acetyl cysteine, co-enzyme Q10, zinc, selenium, folic acid and lycopene were most commonly used. The vitamins’ mechanism of action and reported doses is presented in Tables 1 and 2. Conclusion Antioxidants generally have a favourable effect on male fertility. Further studies are needed to identify the optimal antioxidant regimen that can be used safely and efficiently in clinical practice.
Systemic review of antioxidant types and doses in male infertility: Benefits on semen parameters, advanced sperm function, assisted reproduction and live-birth rate | Request PDF. Available from: https://www.researchgate.net/publication/322218069_Systemic_review_of_antioxidant_types_and_doses_in_male_infertility_Benefits_on_semen_parameters_advanced_sperm_function_assisted_reproduction_and_live-birth_rate
Male Infertility: The Effect of Natural Antioxidants and Phytocompounds on Seminal Oxidative Stress.
Adewoyin M1, Ibrahim M2, Roszaman R3, Isa MLM4, Alewi NAM5, Rafa AAA6, Anuar MNN1.
Abstract: Defective sperm function has been identified as the most common cause of infertility. The objective of this study was to review recent findings on the effects of various antioxidants on male fertility. High amounts of poly unsaturated fatty acid are found in the mammalian spermatozoa membranes, thereby making them susceptible to lipid peroxidation. Although, free radicals and reactive oxygen species (ROS) play major roles in reproduction, they are strongly associated with oxidative stress. Furthermore, factors such as obesity, inflammation, pollutants and cigarette smoking are negatively correlated with spermatogenesis. Endogenous antioxidants system exists to mediate these damages. In a normal physiological state, the seminal plasma contains antioxidant enzyme mechanism that is capable of quenching these ROS as well as protecting the spermatozoa against any likely damage. However, high level of ROS triggered by inflammatory cells and oxidation of fatty acid in obese subjects may down play antioxidant mechanism resulting in oxidative stress. Evaluation of such oxidative stress is the first step in the treatment of male infertility through administration of suitable antioxidant. Notably, antioxidant such as vitamin E and C, carotenoids and carnitine have been found beneficial in restoring a balance between ROS generation and scavenging activities. There are emerging evidences that herbal products can also boost male reproductive functions. Nonetheless, a good lifestyle, regular exercise, avoidance of stress and observing safety rules at work are habits that can reverse male infertility.
https://www.ncbi.nlm.nih.gov/pubmed/28933362
Fertilichron female Research:
A novel and compact review on the role of oxidative stress in female reproduction
Article (PDF Available): in Reproductive Biology and Endocrinology16(1) · December 2018 with 30 Reads
DOI: 10.1186/s12958-018-0391-5
Abstract: In recent years, the study of oxidative stress (OS) has become increasingly popular. In particular, the role of OS on female fertility is very important and has been focused on closely. The occurrence of OS is due to the excessive production of reactive oxygen species (ROS). ROS are a double-edged sword; they not only play an important role as secondary messengers in many intracellular signaling cascades, but they also exert indispensable effects on pathological processes involving the female genital tract. ROS and antioxidants join in the regulation of reproductive processes in both animals and humans. Imbalances between pro-oxidants and antioxidants could lead to a number of female reproductive diseases. This review focuses on the mechanism of OS and a series of female reproductive processes, explaining the role of OS in female reproduction and female reproductive diseases caused by OS, including polycystic ovary syndrome (PCOS), endometriosis, preeclampsia and so on. Many signaling pathways involved in female reproduction, including the Keap1-Nrf2, NF-κB, FOXO and MAPK pathways, which are affected by OS, are described, providing new ideas for the mechanism of reproductive diseases.
(PDF) A novel and compact review on the role of oxidative stress in female reproduction. Available from: https://www.researchgate.net/publication/327132785_A_novel_and_compact_review_on_the_role_of_oxidative_stress_in_female_reproduction?ev=publicSearchHeader&_sg=1WuS5w02ZgK4r2kOKPRJwnzWk0NrvPpKrmEDCCZsxzPWP8vJ7UcbsIusqFAIKbAwmpUf5p-f5mrVMkw
Fertilichron male & female Research:
Pyrroloquinoline quinone prevents oxidative stress-induced neuronal death probably through changes in oxidative status of DJ-1.
Nunome K1, Miyazaki S, Nakano M, Iguchi-Ariga S, Ariga H.
Abstract: Pyrroloquinoline quinone (PQQ) has been shown to play a role as an anti-oxidant in neuronal cells and prevent neuronal cell death in a rodent stroke model. DJ-1, a causative gene product for a familial form of Parkinson's disease, plays a role in anti-oxidative stress function by self-oxidation of DJ-1. In this study, the expression level and oxidation status of DJ-1 were examined in SHSY-5Y cells and primary cultured neurons treated with 6-hydroxydopamine (6-OHDA) or H(2)O(2) in the presence or absence of PQQ. The pI shift of DJ-1 to an acidic point, which was observed in SHSY-5Y cells treated with 6-OHDA, was inhibited by PQQ. TOF-MS analyses showed that while the level of a reduced form of DJ-1, one of the active forms of DJ-1, was decreased in SHSY-5Y cells treated with 6-OHDA or H(2)O(2), PQQ increased the level of the reduced form of DJ-1. These results suggest that PQQ prevents oxidative stress-induced changes in oxidative status of DJ-1. Therefore, the neuroprotective effects of PQQ on oxidative stress-induced neuronal death may be at least in part involved in increased level of an active form of DJ-1.
https://www.ncbi.nlm.nih.gov/pubmed/18591768
Harris CB, Chowanadisai W, Mishchuk DO, Satre MA, Slupsky CM, Rucker RB.
J Nutr Biochem.2013 Dec;24(12):2076-84. doi: 10.1016/j.jnutbio.2013.07.008.
Dietary pyrroloquinoline quinone (PQQ) alters indicators of inflammation and mitochondrial-related metabolism in human subjects.
Abstract: Pyrroloquinoline quinone (PQQ) influences energy-related metabolism and neurologic functions in animals. The mechanism of action involves interactions with cell signaling pathways and mitochondrial function. However, little is known about the response to PQQ in humans. Using a crossover study design, 10 subjects (5 females, 5 males) ingested PQQ added to a fruit-flavored drink in two separate studies. In study 1, PQQ was given in a single dose (0.2 mg PQQ/kg). Multiple measurements of plasma and urine PQQ levels and changes in antioxidant potential [based on total peroxyl radical-trapping potential and thiobarbituric acid reactive product (TBAR) assays] were made throughout the period of 48 h. In study 2, PQQ was administered as a daily dose (0.3 mg PQQ/kg). After 76 h, measurements included indices of inflammation [plasma C-reactive protein, interleukin (IL)-6 levels], standard clinical indices (e.g., cholesterol, glucose, high-density lipoprotein, low-density lipoprotein, triglycerides, etc.) and (1)H-nuclear magnetic resonance estimates of urinary metabolites related in part to oxidative metabolism. The standard clinical indices were normal and not altered by PQQ supplementation. However, dietary PQQ exposure (Study 1) resulted in apparent changes in antioxidant potential based on malonaldehyde-related TBAR assessments. In Study 2, PQQ supplementation resulted in significant decreases in the levels of plasma C-reactive protein, IL-6 and urinary methylated amines such as trimethylamine N-oxide, and changes in urinary metabolites consistent with enhanced mitochondria-related functions. The data are among the first to link systemic effects of PQQ in animals to corresponding effects in humans.
https://www.sciencedirect.com/science/article/pii/S0955286313001599
Zhang J, Meruvu S1, Bedi YS1, Chau J1, Arguelles A1, Rucker R2, Choudhury M3.
Nutr Res.2015 Sep;35(9):844-9. doi: 10.1016/j.nutres.2015.06.014. Epub 2015 Jul 2.
Pyrroloquinoline quinone increases the expression and activity of Sirt1 and -3 genes in HepG2 cells.
Abstract: Sirtuin (Sirt) 1 and Sirt 3 are nicotinamide adenine dinucleotide ((+))-dependent protein deacetylases that are important to a number of mitochondrial-related functions; thus, identification of sirtuin activators is important. Herein, we hypothesize that pyrroloquinoline quinone (PQQ) can act as a Sirt1/Sirt3 activator. In HepG2 cell cultures, PQQincreased the expression of Sirt1 and Sirt3 gene, protein, and activity levels (P < .05). We also observed a significant increase in nicotinamide phosphoribosyltransferase gene expression (as early as 18 hours) and increased NAD(+) activity at 24 hours. In addition, targets of Sirt1 and Sirt3 (peroxisome proliferator-activated receptor γ coactivator 1α, nuclear respiratory factor 1 and 2, and mitochondrial transcription factor A) were increased at 48 hours. This is the first report that demonstrates PQQas an activator of Sirt1 and Sirt3 expression and activity, making it an attractive therapeutic agent for the treatment of metabolic diseases and for healthy aging. Based on our study and the available data in vivo, PQQhas the potential to serve as a therapeutic nutraceutical, when enhancing mitochondrial function.
https://www.ncbi.nlm.nih.gov/pubmed/26275361/
Nakano M, Kawasaki Y, Suzuki N, Takara T.
J Nutr Sci Vitaminol (Tokyo).2015;61(3):233-40. doi: 10.3177/jnsv.61.233.
Effects of Pyrroloquinoline Quinone Disodium Salt Intake on the Serum Cholesterol Levels of Healthy Japanese Adults.
Abstract: Pyrroloquinoline quinone (PQQ) is a water-soluble quinone compound that has a strong anti-oxidant capacity. A previous study in rats fed a PQQ-depleted diet showed that elevated levels of serum triglyceride (TG) decreased after PQQsupplementation. However, there is only one study reporting the effects of PQQon serum lipid levels, such as those of TG and cholesterol, in humans. In this study, the effects of PQQdisodium salt (BioPQQ™) on serum TG and cholesterol levels in humans after 6 and 12 wk of treatment at an oral dosage of 20 mg/d were examined. This trial was conducted according to a randomized, placebo-controlled, double-blinded protocol. A total of 29 healthy Japanese adults, ranging from 40 to 57 y old, with normal to moderately high TG levels (110-300 mg/dL) as measured by a recent blood examination, were included in this study. In eleven volunteers out of 29, serum low-density lipoprotein cholesterol (LDL-chol) levels at baseline were high (≥140 mg/dL). After 12 wk, the mean serum TG levels had not changed; however, a marginally significant decrease in the mean LDL-chol (from 136.1 to 127.0 mg/dL) was observed in the PQQgroup. In the stratification analysis of the high LDL-chol subgroup (baseline LDL-chol level ≥140 mg/dL), the mean LDL-chol levels decreased significantly from the baseline values in the PQQgroup compared to the placebo group. Our study findings suggest that PQQsuppressed the LDL-chol level, which is an important finding, because a high level of this lipid is a risk factor for various lifestyle-related diseases.
Fertilichron male Research:
The Catsper channel and its roles in male fertility: a systematic review.
Sun XH1, Zhu YY2, Wang L3, Liu HL4, Ling Y4, Li ZL4, Sun LB4.
Abstract: The Catsper channel is a sperm-specific, Ca2+-permeable, pH-dependent, and low voltage-dependent channel that is essential for the hyperactivity of sperm flagellum, chemotaxis towards the egg, capacitation and acrosome reaction. All of these physiological events require calcium entry into sperm cells. Remarkably, Catsper genes are exclusively expressed in the testis during spermatogenesis, and are sensitive to ion channel-induced pH change, such as NHEs, Ca2+ATPase, K+ channel, Hv1 channel and HCO3- transporters. Furthermore, the Catsper channel is regulated by some physiological stimulants, such as progesterone, cyclic nucleotides (e.g., cAMP, cGMP), zona pellucida (ZP) glycoproteins and bovine serum albumin (BSA). All of these factors normally stimulate Ca2+ entry into sperm through the Catsper channel. In addition, the Catsper channel may be a potential target for male infertility treatment or contraception. This review will focus on the structure, functions, regulation mechanisms and medicinal targets of the Catsper channel.
https://www.ncbi.nlm.nih.gov/pubmed/28810916
Intracellular Ca2+ threshold reversibly switches flagellar beat off and on.
Sánchez-Cárdenas C1, Montoya F2, Navarrete FA3, Hernández-Cruz A4, Corkidi G2, Visconti PE3, Darszon A1.
Abstract: Sperm motility is essential for fertilization. The asymmetry of flagellar beat in spermatozoa is finely regulated by intracellular calciumconcentration ([Ca2+]i). Recently, we demonstrated that the application of high concentrations (10-20 μM) of the Ca2+ ionophore A23187 promotes sperm immobilization after 10 minutes, and its removal thereafter allows motility recovery, hyperactivation and fertilization. In addition, the same ionophore treatment overcomes infertility observed in sperm from Catsper1-/-, Slo3-/- and Adcy10-/-, but not PMCA4-/-, which strongly suggest that regulation of [Ca2+]i is mandatory for sperm motility and hyperactivation. In this study we found that prior to inducing sperm immobilization, high A23187 concentrations (10 μM) increase flagellar beat. While 5-10 μM A23187 substantially elevates [Ca2+]i and rapidly immobilizes sperm in a few minutes, smaller concentrations (0.5 and 1 μM) provoke smaller [Ca2+]i increases and spermhyperactivation, confirming that [Ca2+]i increases act as a motility switch. Until now the [Ca2+]i thresholds that switch motility on and off were not fully understood. To study the relationship between [Ca2+]i and flagellar beating, we developed an automatic tool that allows the simultaneous measurement of these two parameters. Individual spermatozoa were treated with A23187 which is then washed to evaluate [Ca2+]i and flagellar beat recovery using the implemented method. We observe that [Ca2+]i must decrease below a threshold concentration range to facilitate subsequent flagellar beat recovery and sperm motility.
https://www.ncbi.nlm.nih.gov/pubmed/29893793
Fertilichron female Research:
Proceedings in Obstetrics and Gynecology, 2011 November;2(2):18 Please cite this paper as:
Maassen RA. Calcium and vitamin D for the reproductive female.
Proc Obstet Gynecol. 2011 November;2(2):Article 18 [ 9 p.].
Available from: http://ir.uiowa.edu/pog/. Free full text article. Corresponding author: Rachel A. Maassen, M.D. Department of Obstetrics and Gynecology, University of Iowa, 51212 PFP, 200 Hawkins Drive, Iowa City, IA 52242. Telephone (319)356-3019. rachelmaassen@uiowa.edu. This is an Open Access article distributed under the terms of the Creative Commons Attribution 3.0 Unported License (http://creativecommons.org/licenses/by/3.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited 1 Calcium and vitamin D for the reproductive female Rachel E. Maassen, MD
Abstract: The importance of calcium as well as its interdependence upon vitamin D is well established. Vitamin D acts via the vitamin D receptor, which is found in 37 different human tissues. Because of its rather ubiquitous localization, vitamin D is the topic of a great deal of associative research. However, caution must be exercised in interpreting these initial studies until clear evidence for causality becomes available. The purpose of this article is to review some of the known vitamin D and calcium associations as well as the current guidelines for calcium and vitamin D supplementation in the reproductive female. 1 The Department of Obstetrics and Gynecology, The Carver College of Medicine, The University of Iowa, Iowa City, Iowa, USA
Associations between serum calcium concentration and postpartum health and reproductiveperformance in dairy cows.
Abstract: In the present study, the aim was to evaluate the associations between serum calcium concentration after calving and serum metabolites, postpartum disorders, and reproductive performance in dairy cows. Blood samples were collected from 200 Holstein cows immediately and 1, 2, 4, 6, and 8 weeks after calving to measure serum metabolites and progesterone concentrations. Cows were divided into three groups on the basis of the mean serum calcium concentration after calving: a Low group (<7.9 mg/dL, n = 52), a Moderate group (7.9-9.6 mg/dL, n = 100), and a High group (≥9.7 mg/dL, n = 48). Total cholesterol (TCH) concentration was greater in the High group than in the Moderate group during the postpartum period (P < 0.01). The High group had greater albumin concentrations during the postpartum period (P < 0.01) and glucose concentrations after calving and 1 week postpartum (P < 0.05) than the Low and Moderate groups. The High group had a lesser incidence of retained placenta than the Low (P < 0.1) and Moderate (P < 0.01) groups, and a lesser incidence of clinical endometritis than the Moderate group (P < 0.05). The probability of resuming estrous cyclicity by 8 weeks postpartum was greater in the High group than in the Low group (hazard ratio = 3.71, P < 0.05). In conclusion, greater serum calcium concentration after calving is associated with greater serum TCH, albumin, and glucose concentrations, a lesser incidence of retained placenta, and clinical endometritis, and earlier resumption of estrous cyclicity in dairy cows.
https://www.ncbi.nlm.nih.gov/pubmed/30120012
Assessment of dietary intake and mineral status in pregnant women.
Kocyłowski R1,2, Lewicka I3, Grzesiak M4, Gaj Z1,5, Sobańska A3, Poznaniak J3, von Kaisenberg C6, Suliburska J7.
Abstract:
Purpose: To evaluate the dietary intake of pregnant women and their nutritional status of Ca, Mg, Fe, Zn, and Cu, as the nutritional status of pregnant women is an important factor for the proper progression of a pregnancy and the development and health of the foetus.
Methods: The study was conducted on 108 pregnant women ages 18-42, at 6-32 weeks of gestation. We used a questionnaire and a 24-h recall nutrition interview. Hair samples were taken for testing and the level of each mineral was assessed using atomic absorption spectrometry. The results were analysed using the Dietetyk and Statistica 10 software.
Results: Low levels of Fe, Zn, Ca, Mg, vitamin D, and folic acid intake were seen in the pregnant women, with the use of dietary supplements significantly increasing their intake of Fe, Zn, and folic acid. The concentration of zinc and magnesium in the women's hair was shown to be affected by their age and, in the case of magnesium, by the week of pregnancy.
Conclusions: It was observed that the diet of pregnant women is characterised by low levels of Fe, Zn, Ca, Mg, vitamin D, and folic acid. Dietary supplementation with vitamins and minerals significantly increases the daily Fe and folic acid intake in pregnant women. The concentration of Zn and Mg in hair depends on the age of pregnant women and Mg level in the hair of women decreases during pregnancy.
https://www.ncbi.nlm.nih.gov/pubmed/29541858
Effect of blood ionised calcium concentration at calving on fertility outcomes in dairy cattle.
Mahen PJ1, Williams HJ1, Smith RF1, Grove-White D1.
Abstract: Clinical and subclinical hypocalcaemia are common in dairy cows, yet evidence in the literature assessing their impact on fertility is inconsistent. The aim of this prospective cohort study was to examine associations between blood ionised calcium concentration at calving and fertility outcomes in dairy cattle. Blood samples were taken from 137 Holstein cows from four commercial dairy herds within 24 hours of calving and analysed for blood ionised calcium using an Epocal Point of Care Analyser (Epocal, Ottawa, Canada). Data collected from routine veterinary fertility examinations and herd records were used to investigate the association of ionised calcium with the outcomes: time to first service, time to conception and endometritis. There were significant negative associations between blood ionised calciumconcentration and time to first service (HR 1.33, P=0.001) and blood ionised calcium concentration and time to conception (HR 1.16, P=0.04). There was no significant association between blood ionised calcium concentration and endometritis. The results of this study imply that management policies that minimise the reduction in blood ionised calcium concentration in the periparturient dairy cow are likely to improve reproductive outcomes and should be considered as part of the multifactorial approach to optimising dairy cow fertility.
Fertilichron male Research:
Human Sperm Characteristics with Regard to Cobalt, Chromium, and Lead in Semen and Activity of Catalase in Seminal Plasma
Article: in Biological Trace Element Research · June 2018 with 32 Reads
DOI: 10.1007/s12011-018-1416-9
Abstract: We analyzed cobalt (Co), chromium (Cr), and lead (Pb) concentrations in human semen and catalase CAT activity in seminal plasma and the effects of their relations on the sperm quality. We obtained semen samples from men (n = 168) undergoing routine infertility evaluation. Studies included two groups based on the ejaculate parameters: I (n = 39; normal ejaculate; normozoospermia); II (n = 129; pathological spermiogram). We examined relationships and differences between Co, Cr, and Pb concentrations in seminal plasma, CAT activity, and semen parameters. We did not establish differences in Co, Cr, and Pb concentrations and CAT activity from men between normozoospermic and those with pathological spermiogram. We found a significantly lower Co concentration and CAT activity in males with normal sperm motility than in asthenozoospermic males. We found significantly lower Co and a higher Pb concentration in males with normal morphology of spermatozoa than in teratozoospermic males. We found a significantly higher Pb concentration in the individuals with consumption of alcohol than in those without consumption. There were significant correlations between Co and Pb concentrations, sperm progressive motility (A + B, i.e., fast and slow progressive motility; Co-negatively; Pb-positively), and normal morphology of spermatozoa (Co-negatively; Pb-positively). We found a significant negative correlation between Cr concentration and slow progressive motility, and between CAT activity and volume of ejaculate. Co, Cr, and Pb levels and CAT activity were related to sperm characteristics and male fertility. The impact of alcohol may be manifested by a disturbance in Pb equilibrium in the body. Co and Pb influence progressive motility and normal morphology of human spermatozoa. Thus, Co and Pb levels in semen may be a useful diagnostic in male infertility. Most of the results of this study are in contrast to expectations. Namely, Pb is a toxic element and its harmful effects (poor semen quality) may be expected already at relatively low level of Pb exposure and are particularly visible with increasing of Pb. Co and Cr(III) are essential elements and harmful effects may be expected at their deficiency and/or overexposure.
Human Sperm Characteristics with Regard to Cobalt, Chromium, and Lead in Semen and Activity of Catalase in Seminal Plasma | Request PDF. Available from: https://www.researchgate.net/publication/326076599_Human_Sperm_Characteristics_with_Regard_to_Cobalt_Chromium_and_Lead_in_Semen_and_Activity_of_Catalase_in_Seminal_Plasma?ev=publicSearchHeader&_sg=sxk_q2ObQlTtjItk91WnPwBpQRBExHIAwzdkke5yrn_fpULVOnWxC54S1U6Qbg4k9zCruBfQUH4MeTM
Fertilichron female Research:
Role of reducing fertility factors in reproductive aged women and their assosiation with micronutrients
Article · October 2016 with 2 Reads
DOI: 10.18370/2309-4117.2016.31.40-48
Abstract: Fertility is ability of sexually mature organism to reproduce offspring. Infertility is an inability of organism to conceive a mature. The frequency of male and female factors is above 40% in the structure of marriage infertility, 15% of infertility causes is caused by both partners, 5–10% of cases are not established. The most common causes of female infertility are an ovulation disorders (25–30%) and tubal occlusion (20–25%). Stress is one of the probable cases of the fertility decline and insufficient effectiveness of the reproductive programs, especially for unknown origin. Hypothalamic-pituitary-adrenal system, which leads to stress reaction, can significantly inhibit the function of the female reproductive system at different levels. Oxidative stress in the ovaries is another important mechanism to reduce fertility. No one doubts that a deficiency of vitamins and elements can reduce fertility and cause infertility. Since impaired fertility involved a number of known active substances, during the infertility treatment should take into account this factor and to include those macro- and microelements and vitamins, the probability of which deficiency is the highest. They include homocysteine, folate, vitamin E, vitamin C, group B vitamins, L-arginine, magnesium, zinc, selenium, and others. According to many publications appointment of the trace elements and vitamins, which are lacking in the body, provides the adaptation of the nervous system, hormonal homeostasis and the optimal condition of the reproductive system organs prior to pregnancy. Physician should be carefully weighed hormone therapy at the fertile period of woman, based on the benefits and risks for the woman and for the unborn child. This hormonal therapy, as a necessary component in patients with endocrine infertility or women in program of assisted reproductive technologies may not have the expected success due to the formation of micronutrient deficiency.
Role of reducing fertility factors in reproductive aged women and their assosiation with micronutrients. Available from: https://www.researchgate.net/publication/312248124_Role_of_reducing_fertility_factors_in_reproductive_aged_women_and_their_assosiation_with_micronutrients
Trace Element Deficiencies and Fertility in Ruminants: A Review
Article · Literature Review in Journal of Dairy Science 62(8):1195-206 · September 1979 with 204 Reads
DOI: 10.3168/jds.S0022-0302(79)83400-1 · Source: PubMed
Abstract: Various minerals (copper, cobalt, selenium, manganese, iodine, zinc, and iron) can influence reproductive performance of ruminants. Reproductive failure may be induced by deficiencies of single or combined trace elements and by imbalances. This review is focused on maladjustments of trace elements leading to impaired breeding performance. Opinion is diverse as to the existence of various reproductive disturbances from either a severe copper depletion or a marginal dietary copper deficiency. Field experience suggests that administration of cobalt to ruminants on cobalt-deficient diets improves their impaired breeding performance. Selenium infertility in ewes is more prevalent in some areas and in some seasons, but the actual cause of this malady and the continuing role of additional factors are unknown. Manganese is necessary for normal fertility in ruminants, and feeding low-manganese rations depresses conception rates. Lack of iodine impairs thyroid activity and also ovarian function. Reproductive failure in the female and in spermatogenesis are manifestations of zinc deficiency. Despite forages rich in iron, low availability in certain instances could affect adversely ruminant reproduction. Knowledge of biochemical dysfunctions from trace element deficiencies is essential to determine the role which trace elements play in fertility of ruminant animals.
Trace Element Deficiencies and Fertility in Ruminants: A Review. Available from: https://www.researchgate.net/publication/22753545_Trace_Element_Deficiencies_and_Fertility_in_Ruminants_A_Review?_sg=ePG6R0QZjJ37LsndCHejvoTla3L0VHCkKnJwx_I6pOuSAsRj0d7MTwZ4B5HPSq3R7HDSDeqVY0IsDFs
Fertilichron male Research:
Multivitamin and micronutrient treatment improves semen parameters of azoospermic patients with maturation arrest
(n=35, double blind, placebo controlled trail for 3 month).
Singh AKet al., Indian J Physiol Pharmacol 2010
Abstract: The study was undertaken to evaluate the efficacy of multivitamin and micronutrient supplementation in azoospermic patients with maturation arrest. A total of 35 azoospermic patients showing maturation arrest on testicular biopsy were recruited in this study. The patients were divided into two groups. Untreated group (n=11) without any treatment and treated group (n=24) who received multivitamins, micronutrients and co-enzyme Q10. The sperm concentration, motility and morphology were evaluated at monthly interval. The results showed reduction in liquefaction time and relative viscosity of the semen in the treated group . Further, in treated group there was appearance of spermatozoa (4.0 million/ml) exhibiting progressive motility (7%) and normal morphology (6%), even in the first follow up visit. The sperm count, motility and normal morphology increased significantly on subsequent visits. Within 3 months (3 visits) 2 pregnancies were reported. These observations indicate that multivitamin and micronutrient supplementation improve the qualitative and quantitative parameters of seminogram in patients with azoospermia of maturation arrest.
Fertilichron female Research:
Assessment of dietary intake and mineral status in pregnant women.
Kocyłowski R1,2, Lewicka I3, Grzesiak M4, Gaj Z1,5, Sobańska A3, Poznaniak J3, von Kaisenberg C6, Suliburska J7.
Abstract:
Purpose: To evaluate the dietary intake of pregnant women and their nutritional status of Ca, Mg, Fe, Zn, and Cu, as the nutritional status of pregnant women is an important factor for the proper progression of a pregnancy and the development and health of the foetus.
Methods: The study was conducted on 108 pregnant women ages 18-42, at 6-32 weeks of gestation. We used a questionnaire and a 24-h recall nutrition interview. Hair samples were taken for testing and the level of each mineral was assessed using atomic absorption spectrometry. The results were analysed using the Dietetyk and Statistica 10 software.
Results: Low levels of Fe, Zn, Ca, Mg, vitamin D, and folic acid intake were seen in the pregnant women, with the use of dietary supplements significantly increasing their intake of Fe, Zn, and folic acid. The concentration of zinc and magnesium in the women's hair was shown to be affected by their age and, in the case of magnesium, by the week of pregnancy.
Conclusions: It was observed that the diet of pregnant women is characterised by low levels of Fe, Zn, Ca, Mg, vitamin D, and folic acid. Dietary supplementation with vitamins and minerals significantly increases the daily Fe and folic acid intake in pregnant women. The concentration of Zn and Mg in hair depends on the age of pregnant women and Mg level in the hair of women decreases during pregnancy.
https://www.ncbi.nlm.nih.gov/pubmed/29541858
Role of reducing fertility factors in reproductive aged women and their assosiation with micronutrients
Article: · October 2016 with 2 Reads
DOI: 10.18370/2309-4117.2016.31.40-48
Abstract: Fertility is ability of sexually mature organism to reproduce offspring. Infertility is an inability of organism to conceive a mature. The frequency of male and female factors is above 40% in the structure of marriage infertility, 15% of infertility causes is caused by both partners, 5–10% of cases are not established. The most common causes of female infertility are an ovulation disorders (25–30%) and tubal occlusion (20–25%). Stress is one of the probable cases of the fertility decline and insufficient effectiveness of the reproductive programs, especially for unknown origin. Hypothalamic-pituitary-adrenal system, which leads to stress reaction, can significantly inhibit the function of the female reproductive system at different levels. Oxidative stress in the ovaries is another important mechanism to reduce fertility. No one doubts that a deficiency of vitamins and elements can reduce fertility and cause infertility. Since impaired fertility involved a number of known active substances, during the infertility treatment should take into account this factor and to include those macro- and microelements and vitamins, the probability of which deficiency is the highest. They include homocysteine, folate, vitamin E, vitamin C, group B vitamins, L-arginine, magnesium, zinc, selenium, and others. According to many publications appointment of the trace elements and vitamins, which are lacking in the body, provides the adaptation of the nervous system, hormonal homeostasis and the optimal condition of the reproductive system organs prior to pregnancy. Physician should be carefully weighed hormone therapy at the fertile period of woman, based on the benefits and risks for the woman and for the unborn child. This hormonal therapy, as a necessary component in patients with endocrine infertility or women in program of assisted reproductive technologies may not have the expected success due to the formation of micronutrient deficiency.
Role of reducing fertility factors in reproductive aged women and their assosiation with micronutrients. Available from: https://www.researchgate.net/publication/312248124_Role_of_reducing_fertility_factors_in_reproductive_aged_women_and_their_assosiation_with_micronutrients
Trace Element Deficiencies and Fertility in Ruminants: A Review
Article · Literature Review in Journal of Dairy Science 62(8):1195-206 · September 1979 with 204 Reads
DOI: 10.3168/jds.S0022-0302(79)83400-1 · Source: PubMed
Abstract: Various minerals (copper, cobalt, selenium, manganese, iodine, zinc, and iron) can influence reproductive performance of ruminants. Reproductive failure may be induced by deficiencies of single or combined trace elements and by imbalances. This review is focused on maladjustments of trace elements leading to impaired breeding performance. Opinion is diverse as to the existence of various reproductive disturbances from either a severe copper depletion or a marginal dietary copper deficiency. Field experience suggests that administration of cobalt to ruminants on cobalt-deficient diets improves their impaired breeding performance. Selenium infertility in ewes is more prevalent in some areas and in some seasons, but the actual cause of this malady and the continuing role of additional factors are unknown. Manganese is necessary for normal fertility in ruminants, and feeding low-manganese rations depresses conception rates. Lack of iodine impairs thyroid activity and also ovarian function. Reproductive failure in the female and in spermatogenesis are manifestations of zinc deficiency. Despite forages rich in iron, low availability in certain instances could affect adversely ruminant reproduction. Knowledge of biochemical dysfunctions from trace element deficiencies is essential to determine the role which trace elements play in fertility of ruminant animals.
Trace Element Deficiencies and Fertility in Ruminants: A Review. Available from: https://www.researchgate.net/publication/22753545_Trace_Element_Deficiencies_and_Fertility_in_Ruminants_A_Review?_sg=ePG6R0QZjJ37LsndCHejvoTla3L0VHCkKnJwx_I6pOuSAsRj0d7MTwZ4B5HPSq3R7HDSDeqVY0IsDFs
The effect of micronutrient supplements on female fertility.
Abstract:
Purpose of Review: Benefit of micronutrient supplementation on female fertility.
Recent Findings: Reports of randomized trials are rare. Most studies are focused on multivitamin supplementations. For some micronutrients, a positive impact on fertility could be shown. This article reviews the available clinical studies as well as the pathophysiological background of possible effects and summarizes the potential benefits of selected micronutrients on female fertility.
Summary: Apart from lowering the malformation risk by periconceptional supplementation of folic acid, substitution with different micronutrients, particularly folic acid, vitamin B6, vitamin C, vitamin D, vitamin E, iodine, selenium, iron, and DHA might have a positive impact on infertility treatment. The multivitamin formulation should take the pathophysiology, clinical studies, and upper limits into account.
Fertilichron male Research:
Coenzyme Q10 levels in idiopathic and varicocele-associated asthenozoospermia
(n=82, epidemiological study).
Balercia Get al., Andrologia 2002
Levels of coenzyme Q10 (CoQ10) and of its reduced and oxidized forms (ubiquinol, QH2, and ubiquinone, Qox) have been determined in sperm cells and seminal plasma of idiopathic (IDA) and varicocele‐associated (VARA) asthenozoospermic patients and of controls. The results have shown significantly lower levels of coenzyme Q10 and of its reduced form, QH2, in semen samples from patients with asthenospermia; furthermore, the coenzyme Q10 content was mainly associated with spermatozoa. Interestingly, sperm cells from IDA patients exhibited significantly lower levels of CoQ10 and QH2 when compared to VARA ones. The QH2/Qox ratio was significantly lower in sperm cells from IDA patients and in seminal plasma from IDA and VARA patients when compared with the control group. The present data suggest that the QH2/Qox ratio may be an index of oxidative stress and its reduction, a risk factor for semen quality. Therefore, the present data could suggest that sperm cells, characterized by low motility and abnormal morphology, have low levels of coenzyme Q10. As a consequence, they could be less capable in dealing with oxidative stress which could lead to a reduced QH2/Qox ratio. Furthermore, the significantly lower levels of CoQ10 and QH2 levels in sperm cells from IDA patients, when compared to VARA ones, enable us to hypothesize a pathogenetic role of antioxidant impairment, at least as a cofactor, in idiopathic forms of asthenozoospermia.
https://onlinelibrary.wiley.com/doi/abs/10.1046/j.0303-4569.2001.00485.x
Coenzyme Q10 and male infertility
(n=82, open trail per 26 weeks).
Balercia Get al., J Endocrinol Invest 2009
We had previously demonstrated that Coenzyme Q10 [(CoQ10) also commonly called ubiquinone] is present in well-measurable levels in human seminal fluid, where it probably exerts important metabolic and antioxidant functions; seminal CoQ10 concentrations show a direct correlation with seminal parameters (count and motility). Alterations of CoQ10 content were also shown in conditions associated with male infertility, such as asthenozoospermia and varicocele (VAR). The physiological role of this molecule was further clarified by inquiring into its variations in concentrations induced by different medical or surgical procedures used in male infertility treatment. We therefore evaluated CoQ10 concentration and distribution between seminal plasma and spermatozoa in VAR, before and after surgical treatment, and in infertile patients after recombinant human FSH therapy. The effect of CoQ10 on sperm motility and function had been addressed only through some in vitro experiments. In two distinct studies conducted by our group, 22 and 60 patients affected by idiopathic asthenozoospermia were enrolled, respectively. CoQ10 and its reduced form, ubiquinol, increased significantly both in seminal plasma and sperm cells after treatment, as well as spermatozoa motility. A weak linear dependence among the relative variations, at baseline and after treatment, of seminal plasma or intracellular CoQ10, ubiquinol levels and kinetic parameters was found in the treated group. Patients with lower baseline value of motility and CoQ10 levels had a statistically significant higher probability to be responders to the treatment. In conclusion, the exogenous administration of CoQ10 increases both ubiquinone and ubiquinol levels in semen and can be effective in improving sperm kinetic features in patients affected by idiopathic asthenozoospermia.
(PDF) Coenzyme Q(10) and male infertility. Available from: https://www.researchgate.net/publication/26279045_Coenzyme_Q10_and_male_infertility
Efficacy of coenzyme Q10 on semen parameters, sperm function and reproductive hormones in infertile men
(n=212, double blind, placebo controlled trail per 26 weeks).
Safarinejad MR, J Urol 2009
We determined the efficacy of coenzyme Q10 supplementation on semen parameters, sperm function and reproductive hormone profiles in infertile men. A total of 212 infertile men with idiopathic oligoasthenoteratospermia were randomly assigned to receive 300 mg coenzyme Q10 (Kaneka, Osaka, Japan) orally daily (106 in group 1) or a similar placebo regimen (106 in group 2) during a 26-week period, followed by a 30-week treatment-free phase. Two semen analyses, acrosome reaction test, immunobead test for antisperm antibody, and determination of resting levels of luteinizing hormone, follicle-stimulating hormone, prolactin, testosterone and inhibin B were done in all participants. Blood and seminal plasma total coenzyme Q10 was also assessed. Significant improvement in sperm density and motility was evident with coenzyme Q10 therapy (each p = 0.01). Using the Kruger classification sperm morphology evaluation revealed an increase in the percent of normal forms in the coenzyme Q10 group (p = 0.07). A positive correlation was found between treatment duration with coenzyme Q10 and sperm count (r = 0.46, p = 0.03) as well as with sperm motility (r = 0.45, p = 0.04) and sperm morphology (r = 0.34, p = 0.04). The coenzyme Q10 group had a significant decrease in serum follicle-stimulating hormone and luteinizing hormone at the 26-week treatment phase (each p = 0.03). By the end of the treatment phase the mean +/- SD acrosome reaction had increased from 14% +/- 8% and 15% +/- 8% to 31% +/- 11% and 16% +/- 10% in the coenzyme Q10 and placebo groups, respectively (p = 0.01). Coenzyme Q10 supplementation resulted in a statistically significant improvement in certain semen parameters. However, further studies are needed to draw a final conclusion and evaluate the effect of coenzyme Q10 supplementation on the pregnancy rate.
Efficacy of Coenzyme Q10 on Semen Parameters, Sperm Function and Reproductive Hormones in Infertile Men | Request PDF. Available from: https://www.researchgate.net/publication/24432346_Efficacy_of_Coenzyme_Q10_on_Semen_Parameters_Sperm_Function_and_Reproductive_Hormones_in_Infertile_Men
Multivitamin and micronutrient treatment improves semen parameters of azoospermic patients with maturation arrest
(n=35, double blind, placebo controlled trail for 3 month).
Singh AKet al., Indian J Physiol Pharmacol 2010
The study was undertaken to evaluate the efficacy of multivitamin and micronutrient supplementation in azoospermic patients with maturation arrest. A total of 35 azoospermic patients showing maturation arrest on testicular biopsy were recruited in this study. The patients were divided into two groups. Untreated group (n=11) without any treatment and treated group (n=24) who received multivitamins, micronutrients and co-enzyme Q10. The sperm concentration, motility and morphology were evaluated at monthly interval. The results showed reduction in liquefaction time and relative viscosity of the semen in the treated group. Further, in treated group there was appearance of spermatozoa (4.0 million/ml) exhibiting progressive motility (7%) and normal morphology (6%), even in the first follow up visit. The sperm count, motility and normal morphology increased significantly on subsequent visits. Within 3 months (3 visits) 2 pregnancies were reported. These observations indicate that multivitamin and micronutrient supplementation improve the qualitative and quantitative parameters of seminogram in patients with azoospermia of maturation arrest.
(PDF) Multivitamin and micronutrient treatment improves semen parameters of azoospermic patients with maturation arrest. Available from: https://www.researchgate.net/publication/49621875_Multivitamin_and_micronutrient_treatment_improves_semen_parameters_of_azoospermic_patients_with_maturation_arrest
Tamoxifen combined with coenzyme Q10 for idiopathic oligoasthenospermia
(n=183, double blind, parallel group trail per 6 month).
Tang KFet al., [2011]
Abstract:
Objective: To investigate the effects of tamoxifen (TMX) combined with coenzyme Q10 (CoQ10) on idiopathic oligoasthenospermia.
Methods: A total of 183 patients with idiopathic oligoasthenospermia were randomly divided into a TMX + CoQ10 group (n = 63), a TMX group (n = 61) and a CoQ10 group (n = 59). At the end of 3 and 6 months of treatment, semen analyses and hormone tests were performed, and the results were compared with those obtained before the treatment.
Results: Compared with the pre-treatment results, the levels of follicle-stimulating hormone (FSH), luteinizing hormone (LH) and testosterone (T) and sperm concentration were significantly elevated in the TMX + CoQ10 and TMX groups (P < 0.05), but showed no significant difference in the CoQ10 group (P > 0.05); sperm motility and morphologically normal sperm were increased significantly in the TMX + CoQ10 and CoQ10 groups (P < 0.05), and slightly in the TMX group but with no statistically significant difference (P > 0.05).
CONCLUSION: Tamoxifen combined with CoQ10 can significantly improve sperm concentration, motility and morphology in patients with idiopathic oligoasthenospermia.
Gvozdjáková A, Kucharská J, Dubravicky J, Mojto V, Singh RB.
Dis Markers.2015;2015:827941. doi: 10.1155/2015/827941. Epub 2015 Feb 25.
Coenzyme Q10, α-tocopherol, and oxidative stress could be important metabolic biomarkers of maleinfertility.
Abstract: Oxidative stress, decreased antioxidant capacity, and impaired sperm mitochondrial function are the main factors contributing to maleinfertility. The goal of the present study was to assess the effect of the per os treatment with Carni-Q-Nol (440 mg L-carnitine fumarate + 30 mg ubiquinol + 75 IU vitamin E + 12 mg vitamin C in each softsule) in infertile men on sperm parameters, concentration of antioxidants (coenzyme Q10, CoQ(10-TOTAL), γ, and α-tocopherols), and oxidative stress in blood plasma and seminal fluid. Forty infertile men were supplemented daily with two or three Carni-Q-Nol softsules. After 3 and 6 months of treatment, improved sperm density was observed (by 48.9% and 80.9%, resp.) and after 3-month treatment the sperm pathology decreased by 25.8%. Concentrations of CoQ(10-TOTAL) (ubiquinone + ubiquinol) and α-tocopherol were significantly increased and the oxidative stress was decreased. In conclusion, the effect of supplementary therapy with Carni-Q-Nol showed benefits on sperm function in men, resulting in 45% pregnancies of their women. We assume that assessment of oxidative stress, CoQ(10-TOTAL), and α-tocopherol in blood plasma and seminal fluid could be important metabolic biomarkers in both diagnosis and treatment of maleinfertility.
https://www.ncbi.nlm.nih.gov/pubmed/25810566
Biofactors.2011 Sep-Oct;37(5):374-80. doi: 10.1002/biof.164. Epub 2011 Oct 11.
Coenzyme Q(10) in maleinfertility: physiopathology and therapy.
Abstract: Both the bioenergetic and the antioxidant role of CoQ(10) suggest a possible involvement in sperm biochemistry and maleinfertility. CoQ(10) can be quantified in seminal fluid, where its concentration correlates with sperm count and motility. It was found that distribution of CoQ(10) between sperm cells and seminal plasma was altered in varicocele patients, who also presented a higher level of oxidative stress and lower total antioxidant capacity. The effect of vericocelectomy on partially reversing these biochemical abnormalities is discussed. The redox status of coenzyme Q(10) in seminal fluid was also determined: an inverse correlation was found between ubiquinol/ubiquinone ratio and hydroperoxide levels and between this ratio and the percentage of abnormal sperm forms. After the first in vitro observations CoQ(10) was administered to infertile patients affected by idiopathic asthenozoospermia, originally in an open label study and then in three randomized placebo-controlled trials; doses were around 200-300 mg/day and treatment lasted 6 months. A significant increase in the concentration of CoQ(10) was found, both in seminal plasma and sperm cells. Treatment also led to a certain improvement in sperm motility. In one of the studies there was also a decrease in plasma levels of follicle stimulating horhone (FSH) and luteinizine horhone (LH). Administration of CoQ(10) may play a positive role in the treatment of asthenozoospermia, possibly related to not only to its function in the mitochondrial respiratory chain but also to its antioxidant properties. Further studies are needed in order to determine whether there is also an effect on fertilityrate.
https://iubmb.onlinelibrary.wiley.com/doi/pdf/10.1002/biof.164
Nadjarzadeh A, Shidfar F, Amirjannati N, Vafa MR, Motevalian SA, Gohari MR, Nazeri Kakhki SA, Akhondi MM, Sadeghi MR.
Andrologia.2014 Mar;46(2):177-83. doi: 10.1111/and.12062. Epub 2013 Jan 7.
Effect of Coenzyme Q10supplementation on antioxidant enzymes activity and oxidative stress of seminal plasma: a double-blind randomised clinicaltrial.
Abstract: Low seminal plasma concentrations of coenzyme Q10 (CoQ10) have been correlated with impaired sperm parameters, but the exact mechanism remains of dominating interest. This randomised, placebo-controlled study examined the effect of CoQ10 on catalase, superoxide dismutase (SOD) and F2 -isoprostanes in seminal plasma in infertile men and their relation with CoQ10 concentration. Sixty infertile men with idiopathic oligoasthenoteratozoospermia (OAT) were randomised to receive 200 mg d(-1) of CoQ10 or placebo for 3 months. 47 persons of them completed the study. Semen analysis, anthropometric measurements, diet and physical activity assessment were performed for subjects before and after treatment. Independent and paired t-test, chi-square test and ancova were compared outcomes of supplementation between two groups. CoQ10 levels increased from 44.74 ± 36.47 to 68.17 ± 42.41 ng ml(-1) following supplementation in CoQ10 (P < 0.001). CoQ10 group had higher catalase and SOD activity than the placebo group. There was a significant positive correlation between CoQ10 concentration and normal spermmorphology (P = 0.037), catalase (P = 0.041) and SOD (P < 0.001). Significant difference was shown between the mean of changes in seminal plasma 8-isoprostane in two groups (P = 0.003) after supplementation. Three-month supplementation with CoQ10 in OAT infertile men can attenuate oxidative stress in seminal plasma and improve semen parameters and antioxidant enzymes activity.
A post-publication analysis of the idealized upper reference value of 2.5 mIU/L for TSH: Time to support the thyroid axis with magnesium and iron especially in the setting of reproduction medicine.
Abstract: Laboratory medicine approaches the evaluation of thyroid function mostly through the single determination of the blood level of thyroid stimulating hormone (TSH). Some authors have suggested an upper reference value for TSH of 2.5 mIU/L. This suggestion has not been confirmed by recent clinical studies. These studies have delivered a clinically valid reference range going from 0.3 to 3.5 mIU/L. These values are valid for both for the general population as well as in the setting of fertility and pregnancy. Current biochemical evidence about the elements required to maintain thyroid function shows that these not only include dietary iodine but also magnesium, iron, selenium and coenzyme Q10. Iron is important for the synthesis of thyroid peroxidase; magnesium-ATP contributes to the active process of iodine uptake; iodine has to be sufficiently present in the diet; selenium acts through selenoproteins to protect the thyroid cell during hormone synthesis and in deiodination of thyroxine; coenzyme Q10 influences thyroid vascularity. As a consequence, good clinical practice requires additional biochemical information on the blood levels of magnesium, selenium, coenzyme Q10 as well as iron status. Since these elements are also important for the maintenance of reproductive function, we postulate that they constitute the connecting link between both endocrine systems.
https://www.ncbi.nlm.nih.gov/pubmed/28409122
Lipovac M, Bodner F, Imhof M, Chedraui P.
Reprod Biol Endocrinol.2016 Dec 9;14(1):84.
Comparison of the effect of a combination of eight micronutrients versus a standard mono preparation on sperm parameters.
Abstract:
Background: There are reports showing that l-carnitine alone or in combination with other micronutrients improve sperm parameters. However, comparative studies are still lacking. This study was carried out to compare the short term effects of a combination of eight micronutrients including l-carnitine vs. a mono-substance (l-carnitine alone) on sperm parameters.
Methods: This was a prospective, open-labelled, nonrandomized study that included male subjects (20 to 60 years) with at least 1 year of subfertility and at least one pathological semen analysis who received 3 months treatment with a mono-substance (500 mg l-carnitine/twice a day, n = 156) or a combined compound (440 mg l-carnitine + 250 mg l-arginine + 40 mg zinc + 120 mg vitamin E + 80 mg glutathione + 60 μg selenium + 15 mg coenzyme Q10 + 800 μg folic acid/once a day, n = 143) for the same time period. Sperm parameters were analyzed before and after treatment and groups comparisons performed.
Results: Baseline characteristics were similar among studied groups (age and body mass indices). Semen parameters (volume, density, overall progressive motility [including slow and fast motility]) and percentage of sperm with normal morphology improved after 3 months in both groups as compared to baseline. However, relative change (expressed as % increase of absolute values) for sperm density and overall progressive motility (including fast motility) was found to be higher for the combined micronutrient treatment group as compared to the mono-treatment using l-carnitine alone.
Conclusion: Both analyzed groups displayed a positive short term effect on all sperm parameters; however effect on density and motility was significantly better for the combined formulation. There is need for more research in this matter that includes long term outcome data.
Fertilichron female Research:
Positive correlation between maternal serum coenzyme Q10 levels and infant birth weight.
Haruna M1, Matsuzaki M, Ota E, Honda Y, Tanizaki T, Sekine K, Tabata N, Yeo S, Murashima S.
Abstract:
The purpose of this study was to examine the relationship between the level of maternal serum coenzyme Q10 (CoQ10), which is a lipid-soluble antioxidant, maternal body weight gain, fat mass gain, and infant birth weight. A longitudinal observational study was conducted with 50 healthy pregnant women (average age: 31.1 years, average body mass index (BMI): 21.3 kg/m(2) at prepregnancy) at each trimester. CoQ10 levels were measured by high performance liquid chromatography. Maternal weight and body composition were measured by a bioelectrical impedance analysis. The CoQ10 levels significantly increased throughout pregnancy from the first trimester to the third trimester (P < 0.001), and correlated with not only the serum cholesterol levels (P < 0.01) but also with the serum acetoacetic acid levels (P < 0.05) in the third trimester. The CoQ10 levels correlated with the maternal weight gain (P < 0.05) and fat mass gain (P < 0.05) from the second to the third trimester, after adjusting for lipid markers, age, and smoking habits. The level of CoQ10 during the third trimester was also significantly associated with the infant birth weight (P < 0.05) after adjusting for gestational age, maternal prepregnancy BMI, and smoking habits. Therefore, it is concluded that the level of maternal CoQ10 is positively associated with fetal growth, balancing rapid metabolic changes in the last half of a normal pregnancy.
https://www.ncbi.nlm.nih.gov/pubmed/20641057
Antioxidants for female subfertility.
Showell MG1, Mackenzie-Proctor R, Jordan V, Hart RJ.
Abstract:
Background: A couple may be considered to have fertility problems if they have been trying to conceive for over a year with no success. This may affect up to a quarter of all couples planning a child. It is estimated that for 40% to 50% of couples, subfertility may result from factors affecting women. Antioxidants are thought to reduce the oxidative stress brought on by these conditions. Currently, limited evidence suggests that antioxidants improve fertility, and trials have explored this area with varied results. This review assesses the evidence for the effectiveness of different antioxidants in female subfertility.
Objectives: To determine whether supplementary oral antioxidants compared with placebo, no treatment/standard treatment or another antioxidant improve fertility outcomes for subfertile women.
Search Methods: We searched the following databases (from their inception to September 2016) with no language or date restriction: Cochrane Gynaecology and Fertility Group (CGFG) specialised register, the Cochrane Central Register of Studies (CENTRAL CRSO), MEDLINE, Embase, PsycINFO, CINAHL and AMED. We checked reference lists of appropriate studies and searched for ongoing trials in the clinical trials registers.
Selection Criteria: We included randomised controlled trials (RCTs) that compared any type, dose or combination of oral antioxidant supplement with placebo, no treatment or treatment with another antioxidant, among women attending a reproductive clinic. We excluded trials comparing antioxidants with fertility drugs alone and trials that only included fertile women attending a fertility clinic because of male partner infertility.
Data Collection and Analysis: Two review authors independently selected eligible studies, extracted the data and assessed the risk of bias of the included studies. The primary review outcome was live birth; secondary outcomes included clinical pregnancy rates and adverse events. We pooled studies using a fixed-effect model, and calculated odds ratios (ORs) with 95% confidence intervals (CIs) for the dichotomous outcomes of live birth, clinical pregnancy and adverse events. We assessed the overall quality of the evidence by applying GRADE criteria.
Main Results: We included 50 trials involving 6510 women. Investigators compared oral antioxidants, including combinations of antioxidants, N-acetyl-cysteine, melatonin, L-arginine, myo-inositol, D-chiro-inositol, carnitine, selenium, vitamin E, vitamin B complex, vitamin C, vitamin D+calcium, CoQ10, pentoxifylline and omega-3-polyunsaturated fatty acids versus placebo, no treatment/standard treatment or another antioxidant.Very low-quality evidence suggests that antioxidants may be associated with an increased live birth rate compared with placebo or no treatment/standard treatment (OR 2.13, 95% CI 1.45 to 3.12, P > 0.001, 8 RCTs, 651 women, I2 = 47%). This suggests that among subfertile women with an expected live birth rate of 20%, the rate among women using antioxidants would be between 26% and 43%.Very low-quality evidence suggests that antioxidants may be associated with an increased clinical pregnancy rate compared with placebo or no treatment/standard treatment (OR 1.52, 95% CI 1.31 to 1.76, P < 0.001, 26 RCTs, 4271 women, I2 = 66%). This suggests that among subfertile women with an expected clinical pregnancy rate of 22%, the rate among women using antioxidants would be between 27% and 33%. Heterogeneity was moderately high.There was insufficient evidence to determine whether there was a difference between the groups in rates of miscarriage (OR 0.79, 95% CI 0.58 to 1.08, P = 0.14, 18 RCTs, 2834 women, I2 = 23%, very low quality evidence). This suggests that, among subfertile women with an expected miscarriage rate of 7%, use of antioxidants would be expected to result in a miscarriage rate of between 4% and 7%. There was also insufficient evidence to determine whether there was a difference between the groups in rates of multiple pregnancy (OR 1.00, 95% CI 0.73 to 1.38, P = 0.98, 8 RCTs, 2163 women, I2 = 4%, very low quality evidence). This suggests that among subfertile women with an expected multiple pregnancy rate of 8%, use of antioxidants would be expected to result in a multiple pregnancy rate between 6% and 11%. Likewise, there was insufficient evidence to determine whether there was a difference between the groups in rates of gastrointestinal disturbances (OR 1.55, 95% CI 0.47 to 5.10, P = 0.47, 3 RCTs, 343 women, I2 = 0%, very low quality evidence). This suggests that among subfertile women with an expected gastrointestinal disturbance rate of 2%, use of antioxidants would be expected to result in a rate between 1% and 11%. Overall adverse events were reported by 35 trials in the meta-analysis, but there was insufficient evidence to draw any conclusions.Only one trial reported on live birth, clinical pregnancy or adverse effects in the antioxidant versus antioxidant comparison, and no conclusions could be drawn.Very low-quality evidence suggests that pentoxifylline may be associated with an increased clinical pregnancy rate compared with placebo or no treatment (OR 2.07, 95% CI 1.20 to 3.56, P = 0.009, 3 RCTs, 276 women, I2 = 0%). This suggests that among subfertile women with an expected clinical pregnancy rate of 25%, the rate among women using pentoxifylline would be between 28% and 53%.There was insufficient evidence to determine whether there was a difference between the groups in rates of miscarriage (OR 1.34, 95% CI 0.46 to 3.90, P = 0.58, 3 RCTs, 276 women, I2 = 0%) or multiple pregnancy (OR 0.78, 95% CI 0.20 to 3.09, one RCT, 112 women, very low quality evidence). This suggests that among subfertile women with an expected miscarriage rate of 4%, the rate among women using pentoxifylline would be between 2% and 15%. For multiple pregnancy, the data suggest that among subfertile women with an expected multiple pregnancy rate of 9%, the rate among women using pentoxifylline would be between 2% and 23%.The overall quality of evidence was limited by serious risk of bias associated with poor reporting of methods, imprecision and inconsistency.
Authors' Conclusion: In this review, there was very low-quality evidence to show that taking an antioxidant may provide benefit for subfertile women, but insufficient evidence to draw any conclusions about adverse events. At this time, there is limited evidence in support of supplemental oral antioxidants for subfertile women.
https://www.ncbi.nlm.nih.gov/pubmed/28752910
A post-publication analysis of the idealized upper reference value of 2.5 mIU/L for TSH: Time to support the thyroid axis with magnesium and iron especially in the setting of reproduction medicine.
Abstract: Laboratory medicine approaches the evaluation of thyroid function mostly through the single determination of the blood level of thyroid stimulating hormone (TSH). Some authors have suggested an upper reference value for TSH of 2.5 mIU/L. This suggestion has not been confirmed by recent clinical studies. These studies have delivered a clinically valid reference range going from 0.3 to 3.5 mIU/L. These values are valid for both for the general population as well as in the setting of fertility and pregnancy. Current biochemical evidence about the elements required to maintain thyroid function shows that these not only include dietary iodine but also magnesium, iron, selenium and coenzyme Q10. Iron is important for the synthesis of thyroid peroxidase; magnesium-ATP contributes to the active process of iodine uptake; iodine has to be sufficiently present in the diet; selenium acts through selenoproteins to protect the thyroid cell during hormone synthesis and in deiodination of thyroxine; coenzyme Q10 influences thyroid vascularity. As a consequence, good clinical practice requires additional biochemical information on the blood levels of magnesium, selenium, coenzyme Q10 as well as iron status. Since these elements are also important for the maintenance of reproductive function, we postulate that they constitute the connecting link between both endocrine systems.
Fertilichron male Research:
Does folic acid and zinc sulphate intervention affect endocrine parameters and sperm characteristics in men?
(n=47 fertile, 40 subfertile, double blind, placebo controlled trail per 26 weeks).
Ebisch IMet al., Int J Androl 2006
We evaluated pre‐and post‐intervention endocrine and semen parameters in a double‐blind, placebo‐controlled intervention study to investigate the underlying mechanism of increased sperm concentration after folic acid and zinc sulphate intervention. A total of 47 fertile and 40 subfertile males participated in a 26‐week intervention study consisting of a daily treatment with folic acid (5 mg/day) and zinc sulphate (66 mg/day), or placebo. Pre‐and post‐intervention semen parameters, serum folate, zinc, follicle‐stimulating hormone (FSH), testosterone and inhibin B concentrations were measured. The results indicated that intervention treatment significantly increased sperm concentration in subfertile males. Other semen and endocrine parameters were not affected by intervention treatment. At baseline, positive correlations were found between serum zinc and sperm concentration, motility and inhibin B. Serum zinc and FSH were inversely correlated. As (already) well known from previous research, inhibin B positively correlated with sperm concentration, motility and morphology, and was inversely correlated with FSH. The latter was positively correlated with testosterone. In addition, testosterone and inhibin B were inversely correlated. After intervention, the correlations with zinc disappeared. We conclude that the increase in sperm concentration after folic acid and zinc sulphate intervention is not the result of alterations in FSH, testosterone or inhibin B concentrations. Although zinc and folate have several effects on spermatogenesis, the underlying mechanisms involved are not clear.
https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1365-2605.2005.00598.x
One-carbon cycle support rescues sperm damage in experimentally induced varicocoele in rats.
Mohammadi P1,2, Hassani-Bafrani H2,3, Tavalaee M1, Dattilo M4, Nasr-Esfahani MH1,5.
Abstract:
Objectives: To investigate whether micronutrients in support of the one-carbon cycle and glutathione synthesis are effective in improving sperm damage after surgical varicocoele induction in rats and whether any effect is achieved without a rebound reductive stress as seen with oral antioxidants.
Materials and Methods: Surgical varicocoele was induced in adult male Wistar rats and resulted in significant damage to the testis and sperm cells measured at 2 and 4 months after surgery. At 2 months after surgery, rats received a 2-month oral supplementation in support of the one-carbon cycle containing B vitamins (B2, B3, B6, folic acid and B12), N-acetyl-cysteine, zinc, small amounts of vitamin E, and a natural source of betalains and quercetine (Condensyl® ; Parthenogen SAGL, Lugano, Switzerland and Nurilia SARL, Lyon, France).
Results: One-carbon cycle supplementation, compared to untreated controls, significantly improved the morphometric characteristics of testis (P < 0.05), sperm concentration, motility and abnormal morphology (P < 0.001), sperm chromatin condensation (aniline blue staining, P < 0.05), sperm DNA damage (acridine orange staining, P < 0.05) and sperm lipid peroxidation (BODIPY C11, P < 0.001). The improvement in both nuclear condensation and DNA damage and the lack of excessive inhibition of lipid peroxidation confirmed that no reductive stress had occurred.
Conclusions: Micronutrients in support of the one-carbon cycle are effective in the treatment of surgically induced varicocoele in rats, probably by activating natural antioxidant defences and epigenetics. These results support the idea that essential micronutrients including B vitamins may also have a positive influence in clinical varicocoele, which should be tested in prospective clinical trials.
https://www.ncbi.nlm.nih.gov/pubmed/29752770
Azizollahi G, Azizollahi S, Babaei H, Kianinejad M, Baneshi MR, Nematollahi-mahani SN.
J Assist Reprod Genet.2013 Apr;30(4):593-9. doi: 10.1007/s10815-013-9961-9. Epub 2013 Feb 24.
Effects of supplement therapy on sperm parameters, protamine content and acrosomal integrity of varicocelectomized subjects.
Abstract:
Purpose: Surgical repair of varicocele has long been a procedure to correct spermatogenesis. However, the outcome has been reported to be inadequate. We combined varicocelectomy with supplement therapy to evaluate the concurrent effect of these procedures.
Methods: A prospective randomized controlled study was undertaken to investigate the effects of zinc sulfate, folic acid and zinc sulfate/folic acid on sperm quality, protamine content and acrosomal integrity following surgical repair of varicocele. Male subjects with palpable varicocele were included in the study and randomized into four groups. Subjects received Zinc sulfate, Folic acid, Zinc sulfate/Folic acid or placebo for 6 months. A semen sample was obtained before surgery and 3 and 6 months after surgical repair. Semen samples were evaluated for sperm parameters as well as chromatin content and acrosomal integrity.
Results: Most of the evaluated parameters showed a mild improvement after varicocelectomy in the placebo group. Interestingly, co-administration of Zinc sulfate and folic acid improved most factors significantly. Folic acid administration but not zinc sulfate could increase sperm number. Hence, Zinc sulfate was better than folic acid when change in morphology was assessed, and none of them was significantly effective in sperm motility. In Zinc sulfate and Folic acid groups, protamine content and halo formation rate significantly improved.
Conclusions: We may conclude that co-administration of zinc and folic acid significantly improved sperm parameters and increased varicocelectomy outcomes. So, medical treatment with compatible drugs after surgery might be advantageous for obtaining acceptable results.
Fertilichron female Research:
Folate Metabolism and Human Reproduction.
Abstract:
Folate metabolism affects ovarian function, implantation, embryogenesis and the entire process of pregnancy. In addition to its well-established effect on the incidence of neural tube defects, associations have been found between reduced folic acid levels and increased homocysteine concentrations on the one hand, and recurrent spontaneous abortions and other complications of pregnancy on the other. In infertility patients undergoing IVF/ICSI treatment, a clear correlation was found between plasma folate concentrations and the incidence of dichorionic twin pregnancies. In patients supplemented with 0.4 mg/d folic acid undergoing ovarian hyperstimulation and oocyte pick-up, carriers of the MTHFR 677T mutation were found to have lower serum estradiol concentrations at ovulation and fewer oocytes could be retrieved from them. It appears that these negative effects can be compensated for in full by increasing the daily dose of folic acid to at least 0.8 mg. In carriers of the MTHFR 677TT genotype who receive appropriate supplementation, AMH concentrations were found to be significantly increased, which could indicate a compensatory mechanism. AMH concentrations in homozygous carriers of the MTHFR 677TT genotype could even be overestimated, as almost 20 % fewer oocytes are retrieved from these patients per AMH unit compared to MTHFR 677CC wild-type individuals.
https://www.ncbi.nlm.nih.gov/pubmed/25278626
Possible roles for folic acid in the regulation of trophoblast invasion and placental development in normal early human pregnancy.
Williams PJ1, Bulmer JN, Innes BA, Broughton Pipkin F.
Abstract: In addition to its role in the prevention of neural tube defects, folic acid has many other physiological functions, including cell proliferation, DNA replication, and antioxidant protection. The aim of this study was to determine the role that folic acid has in regulating placental trophoblast development. Placental explants from placentae at gestational age 7 wk (n = 3) were cultured in folic acid at concentrations of 10(-6) M, 10(-8) M, and 10(-10) M. Extravillous trophoblast (EVT) invasion was assessed following 6-day culture, and explants were used for immunohistochemical evaluation of proliferation (MKI67) and apoptosis (active caspase 3). In addition, an array was performed on cell culture supernatants to examine a range of matrix metalloproteinases (MMPs) and tissue inhibitors of MMPs (TIMPs). Folic acid increased the invasion of EVT cells in this explant model by between 83% and 19% (P = 0.005), and this was associated with increased MKI67 positivity and decreased active caspase 3 positivity; this effect was concentration dependent and showed a biphasic response. In addition, culture in folic acid increased vascular density, as determined by anti-CD31 immunostaining (P = 0.05). The increase in EVT invasion correlated with increased placental explant secretion of MMP2 (P = 0.01), MMP3 (P = 0.01), and MMP9 (P = 0.02). This study demonstrates that folic acid is potentially important in a number of crucial early stages of placental development, including EVT invasion, angiogenesis, and secretion of MMPs, and highlights the need for further studies to address the benefit of longer-term folic acid supplementation throughout pregnancy to prevent pregnancy disorders associated with deficient placental development, including preeclampsia.
https://www.ncbi.nlm.nih.gov/pubmed/21349824
Preconception folic acid supplementation and risk for chromosome 21 nondisjunction: a report from the National Down Syndrome Project.
Hollis ND1, Allen EG, Oliver TR, Tinker SW, Druschel C, Hobbs CA, O'Leary LA, Romitti PA, Royle MH, Torfs CP, Freeman SB, Sherman SL, Bean LJ.
Abstract: Both a lack of maternal folic acid supplementation and the presence of genetic variants that reduce enzyme activity in folate pathway genes have been linked to meiotic nondisjunction of chromosome 21; however, the findings in this area of research have been inconsistent. To better understand these inconsistencies, we asked whether maternal use of a folic acid-containing supplement before conception reduces risk for chromosome 21 nondisjunction. Using questionnaire data from the National Down Syndrome Project, a population-based case-control study, we compared the use of folic acid-containing supplements among mothers of infants with full trisomy 21 due to maternal nondisjunction (n = 702) and mothers of infants born with no major birth defects (n = 983). Using logistic regression, adjusting for maternal age, race/ethnicity, and infant age at maternal interview, we found no evidence of an association between lack of folic acid supplementation and maternal nondisjunction among all case mothers (OR = 1.16; 95% CI: 0.90-1.48). In analyses stratified by meiotic stage and maternal age (<35 or ≥35 years), we found an association among older mothers experiencing meiosis II nondisjunction errors (OR = 2.00; 95% CI: 1.08-3.71). These data suggest that lack of folic acid supplementation may be associated specifically with MII errors in the aging oocyte. If confirmed, these results could account for inconsistencies among previous studies, as each study sample may vary by maternal age structure and proportion of meiotic errors.
https://www.ncbi.nlm.nih.gov/pubmed/23401135
Maternal gene polymorphisms involved in folate metabolism as risk factors for Down syndrome offspring in Southern Brazil.
Brandalize AP1, Bandinelli E, Dos Santos PA, Schüler-Faccini L.
Abstract: This study aimed to investigate the role of maternal polymorphisms, as well as their risk genotypes combinations of MTR A2756G, MTRR A66G, CBS 844ins68, and RFC A80G, involved in folate/homocysteine metabolism, as possible risk factors for Down syndrome (DS) in Southern Brazil. A case-control study was conducted with 239~mothers of DS children and 197~control mothers. The investigation of polymorphisms was performed by PCR and PCR-RFLP. The distribution of genotypic variants was similar in both groups when they were analyzed separately. An investigation of combined risk genotypes showed that the risk of having a DS child for one, two or three risk genotypes was 6.23, 6.96 and 5.84 (95%CI 1.48-26.26; 1.69-28.66; 1.37-24.86), respectively. The combined MTRR 66G and MTHFR 677T alleles were significantly more common among mothers of children with DS than among control mothers (OR 1.55; IC 95% 1.03-2.35). The results show that individual polymorphisms studied in this work are not associated with DS; however, the effects of the combined risk genotypes among MTR, MTRR, CBS and RFC genes are considered maternal risk factors for DS offspring in our population.
https://www.ncbi.nlm.nih.gov/pubmed/21045269
A combined supplementation of omega-3 fatty acids and micronutrients (folic acid, vitamin B12) reduces oxidative stress markers in a rat model of pregnancy induced hypertension.
Kemse NG1, Kale AA1, Joshi SR1.
Abstract:
Objectives: Our earlier studies have highlighted that an altered one carbon metabolism (vitamin B12, folic acid, and docosahexaenoic acid) is associated with preeclampsia. Preeclampsia is also known to be associated with oxidative stress and inflammation. The current study examines whether maternal folic acid, vitamin B12 and omega-3 fatty acid supplementation given either individually or in combination can ameliorate the oxidative stress markers in a rat model of pregnancy induced hypertension (PIH).
Materials and Methods: Pregnant Wistar rats were assigned to control and five treatment groups: PIH; PIH + vitamin B12; PIH + folic acid; PIH + Omega-3 fatty acids and PIH + combined micronutrient supplementation (vitamin B12 + folic acid + omega-3 fatty acids). L-Nitroarginine methylester (L-NAME; 50 mg/kg body weight/day) was used to induce hypertension during pregnancy. Blood Pressure (BP) was recorded during pregnancy and dams were dissected at d20 of gestation.
Results: Animals from the PIH group demonstrated higher (p<0.01 for both) systolic and diastolic BP; lower (p<0.01) pup weight; higher dam plasma homocysteine (p<0.05) and dam and offspring malondialdehyde (MDA) (p<0.01), lower (p<0.05) placental and offspring liver DHA and higher (p<0.01) tumor necrosis factor-alpha (TNF-ά) levels as compared to control. Individual micronutrient supplementation did not offer much benefit. In contrast, combined supplementation lowered systolic BP, homocysteine, MDA and placental TNF-ά levels in dams and liver MDA and protein carbonyl in the offspring as compared to PIH group.
Conclusion: Key constituents of one carbon cycle (folic acid, vitamin B12 and DHA) may play a role in reducing oxidative stress and inflammation in preeclampsia.
https://www.ncbi.nlm.nih.gov/pubmed/25405347
The periconceptional period, reproduction and long-term health of offspring: the importance of one-carbon metabolism.
Steegers-Theunissen RP1, Twigt J, Pestinger V, Sinclair KD.
Abstract:
Background: Most reproductive failures originate during the periconceptional period and are influenced by the age and the lifestyle of parents-to-be. We advance the hypothesis that these failures can arise as a partial consequence of derangements to one-carbon (1-C) metabolism (i.e. metabolic pathways that utilize substrates/cofactors such as methionine, vitamin B12, folate). 1-C metabolic pathways drive the synthesis of proteins, biogenic amines and lipids required for early growth, together with the synthesis and methylation of DNA and histones essential for the regulation of gene expression. We review how deficiencies in periconceptional 1-C metabolism affect fertility and development together with underlying mechanisms derived from animal studies. METHODS A literature search was performed using PubMed and bibliographies of all relevant original research articles and reviews. RESULTS We define 'periconception' as a 5-6-month period in women embracing oocyte growth, fertilization, conceptus formation and development to Week 10 of gestation (coinciding with the closure of the secondary palate in the embryo). During this period significant epigenetic modifications to chromatin occur that correspond with normal development. Subtle variations in 1-C metabolism genes and deficiencies in 1-C substrates/cofactors together with poor lifestyle, such as smoking and alcohol consumption, disturb 1-C metabolism and contribute to subfertility and early miscarriage and compromise offspring health. Procedures used in assisted reproduction can also disturb these metabolic pathways and contribute to poor pregnancy outcomes. CONCLUSIONS Evidence presented indicates that parental nutrition and other lifestyle factors during the periconceptional period can affect reproductive performance via 1-C metabolic pathways. This knowledge provides opportunities for treatment and prevention of reproductive failures and future non-communicable diseases.
https://www.ncbi.nlm.nih.gov/pubmed/23959022
The effect of micronutrient supplements on female fertility.
Abstract:
Purpose of Review: Benefit of micronutrient supplementation on female fertility.
Recent Findings: Reports of randomized trials are rare. Most studies are focused on multivitamin supplementations. For some micronutrients, a positive impact on fertility could be shown. This article reviews the available clinical studies as well as the pathophysiological background of possible effects and summarizes the potential benefits of selected micronutrients on female fertility.
Summary: Apart from lowering the malformation risk by periconceptional supplementation of folic acid, substitution with different micronutrients, particularly folic acid, vitamin B6, vitamin C, vitamin D, vitamin E, iodine, selenium, iron, and DHA might have a positive impact on infertility treatment. The multivitamin formulation should take the pathophysiology, clinical studies, and upper limits into account.
https://www.ncbi.nlm.nih.gov/pubmed/23571830
Association between serum folate and vitamin B-12 and outcomes of assisted reproductive technologies.
Gaskins AJ1, Chiu YH2, Williams PL3, Ford JB4, Toth TL5, Hauser R6, Chavarro JE7; EARTH Study Team
Abstract:
Background: Preconceptional folate and vitamin B-12 have been linked to beneficial reproductive outcomes in both natural pregnancies and those after assisted reproductive technology (ART) treatment.
Objective: The objective of the study was to evaluate the associations of serum folate and vitamin B-12 with ART outcomes.
Design: This analysis included a random sample of 100 women (154 ART cycles) participating in a prospective cohort study [Environment and Reproductive Health (EARTH)] at the Massachusetts General Hospital Fertility Center (2007-2013). Serum folate and vitamin B-12 were measured in blood samples collected between days 3 and 9 of treatment. Generalized estimating equations with adjustment for age, BMI, and race were used to evaluate the association of serum folate and vitamin B-12 with ART outcomes.
Results: Women in the highest quartile of serum folate (>26.3 ng/mL) had 1.62 (95% CI: 0.99, 2.65) times the probability of live birth compared with women in the lowest quartile (<16.6 ng/mL). Women in the highest quartile of serum vitamin B-12 (>701 pg/mL) had 2.04 (95% CI: 1.14, 3.62) times the probability of live birth compared with women in the lowest quartile (<439 pg/mL). Suggestive evidence of an interaction was observed; women with serum folate and vitamin B-12 concentrations greater than the median had 1.92 (95% CI: 1.12, 3.29) times the probability of live birth compared with women with folate and vitamin B-12 concentrations less than or equal to the median. This translated into an adjusted difference in live birth rates of 26% (95% CI: 10%, 48%; P = 0.02).
Conclusion: Higher serum concentrations of folate and vitamin B-12 before ART treatment were associated with higher live birth rates among a population exposed to folic acid fortification. This trial was registered at clinicaltrials.gov as NCT00011713.
Fertilichron male & female Research:
Click for Informational Flyer about FruitFlow.
Bioassay-Guided Isolation and HPLC Determination of Bioactive Compound That Relate to the Antiplatelet Activity (Adhesion, Secretion, and Aggregation) from Solanum lycopersicum.
Fuentes E1, Castro R, Astudillo L, Carrasco G, Alarcón M, Gutiérrez M, Palomo I.
Abstract: In seeking the functionality of foodstuff applicable to medicine, ripe tomato fruits were found to show an antiplatelet activity. Therefore, the bioactive compound was isolated, structurally identified, and studied for an inhibitory effects on platelet adhesion, secretion, and aggregation. The concentration of adenosine in ripe tomato fruits (pulp and skin extracts) and its processing by-products (paste and pomace) was determined by reversed-phase high-performance liquid chromatography (HPLC). According to platelet aggregation inhibition induced by ADP, the total extract residual was fractionated by liquid-liquid separation, obtaining aqueous, ethyl acetate and petroleum ether extracts. The aqueous extract was subjected to repeated permeation over sephadex LH-20 and semipreparative TLC. The isolate finally obtained was identified as adenosine on the basis of ESI-MS, (1)H NMR, HPLC, and UV spectra. Adenosine concentration dependently (2.3-457 μM) platelet aggregation inhibited induced by ADP. Also, adenosine present inhibition of platelet secretion and thrombus formation under flow conditions. The quantitative HPLC analysis revealed significant amounts of adenosine in ripe tomato fruits and its processing by-products. From these results, extracts/fractions of ripe tomato fruits and their processing by-products may be referred to as functional food and functional ingredients containing a compound that inhibits platelet function with a potent preventive effect on thrombus formation, as those that occur in stroke.
https://www.ncbi.nlm.nih.gov/pubmed/23227097
Effects of tomato extract on platelet function: a double-blinded crossover study in healthy humans.
O'Kennedy N1, Crosbie L, Whelan S, Luther V, Horgan G, Broom JI, Webb DJ, Duttaroy AK.
Abstract:
Background: Aqueous extracts from tomatoes display a range of antiplatelet activities in vitro. We previously showed that the active components also alter ex vivo platelet function in persons with a high response to ADP agonist.
Objective: The objective was to evaluate the suitability of a tomato extract for use as a dietary supplement to prevent platelet activation.
Design: A randomized, double-blinded, placebo-controlled crossover study was conducted in 90 healthy human subjects selected for normal platelet function. Changes from baseline hemostatic function were measured 3 h after consumption of extract-enriched or control supplements.
Results: Significant reductions in ex vivo platelet aggregation induced by ADP and collagen were observed 3 h after supplementation with doses of tomato extract equivalent to 6 (6TE) and 2 (2TE) tomatoes [3 micromol ADP/L: 6TE (high dose), -21.3%; 2TE (low dose), -12.7%; P < 0.001; 7.5 micromol ADP/L: 6TE, -7.8%, 2TE, -7.6%; P < 0.001; 3 mg collagen/L: 6TE, -17.5%; 2TE, -14.6%; P = 0.007]. No significant effects were observed for control supplements. A dose response to tomato extract was found at low levels of platelet stimulation. Inhibition of platelet function was greatest in a subgroup with the highest plasma homocysteine (P < 0.05) and C-reactive protein concentrations (P < 0.001).
Conclusion: As a functional food or dietary supplement, tomato extract may have a role in primary prevention of cardiovascular disease by reducing platelet activation, which could contribute to a reduction in thrombotic events.
Fertilichron male Research:
EFFECT OF GRAPE SEED OIL ON ALTERATIONS OF HEMATOLOGICAL PARAMETERS AND SEMEN FLUID QUALITY INDUCED BY DIAZINON IN MALE RATS
Article (PDF Available) · January 2016 with 37 Reads
Abstract: Diazinon (DZN) is one of the organophosphorus (OP) insecticides widely used in local market, can affect animals even after exposure to a single dose. Grape seed oil (GSO), may be rich in more efficient antioxidants. Therefore, the aim of this study was conducted to evaluate the possible protective effect of grapes seed oil GSO in male rats exposed to diazinon at dose of DZN (50 mg/L) induced adverse effects on haematological and semen quality of male rats. The experimental 24 male albino rats were divided into four groups for 1 month. The rats of the first group were served as control. The experimental animals of the second group were exposed to diazinon (DZN). The animals of the third group were supplemented with grape seed oil and treated with DZN. The rats of the fourth group were supplemented with grape seed oil. Hematological such as Red blood corpuscles (RBC) count, hemoglobin (Hb) concentrations and hematocrit (Hct) showed significant reduction, while the value of white blood corpuscles (WBC) count was statistically increased in rats exposed to DZN. Hematological evaluations were chosen as indicators of DZN toxicity and protective role of grape seed oil. Moreover, the semen quality evaluations of the testis showed that DZN causes several severe alterations. Also, animals were dissected and the reproductive organs (epididymus and testes) were taken to measure fertility indices, oxidative parameters and testicular biomarkers. The results indicated DZN decreased testes and epididymus weights for this dose. This effect was dose-related and should be associated with decline in epididymus sperm count, percent of sperm motility, viability and maturity and increased abnormal sperm morphology.
(PDF) EFFECT OF GRAPE SEED OIL ON ALTERATIONS OF HEMATOLOGICAL PARAMETERS AND SEMEN FLUID QUALITY INDUCED BY DIAZINON IN MALE RATS. Available from: https://www.researchgate.net/publication/312176669_EFFECT_OF_GRAPE_SEED_OIL_ON_ALTERATIONS_OF_HEMATOLOGICAL_PARAMETERS_AND_SEMEN_FLUID_QUALITY_INDUCED_BY_DIAZINON_IN_MALE_RATS?_sg=VwzUjZsVr1iLmbuwvG36Jzs9kfrDArdbArmc6lTDTxpI5uWwruDe4NiyXMCc4rAzRzX2AXpjQQGB0K0
Fertilichron male Research:
Myo-inositol as a male fertility molecule: speed them up!
Condorelli RA1, La Vignera S, Mongioì LM, Vitale SG, Laganà AS, Cimino L, Calogero AE.
Abstract: Myo-inositol (MYO) usually represents a therapeutic option for female infertility associated with insulin resistance. Recently, several evidences are accumulating about the potential use of MYO for the treatment of male infertility. This article summarizes the rationale for MYO in the treatment of male infertility. In particular, it illustrates the potential antioxidant and prokinetic role of MYO, and its importance for the modulation of hormonal regulation. In the final part of the manuscript has been added a proposal for a clinical algorithm reserved for patients with asthenozoospermia, where probably MYO could exert specific pharmacological effects.
https://www.ncbi.nlm.nih.gov/pubmed/28724176
Fertilichron female Research:
Vitrification procedure decreases inositol 1,4,5-trisphophate receptor expression, resulting in low fertility of pig oocytes.
Hirose M1, Kamoshita M, Fujiwara K, Kato T, Nakamura A, Wojcikiewicz RJ, Parys JB, Ito J, Kashiwazaki N.
Abstract: Although cryopreservation of mammalian oocytes is an important technology, it is well known that unfertilized oocytes, especially in pigs, are highly sensitive to low temperature and that cryopreserved oocytes show low fertility and developmental ability. The aim of the present study was to clarify why porcine in vitro matured (IVM) oocytes at the metaphase II (MII) stage showed low fertility and developmental ability after vitrification. In vitro matured cumulus oocyte complexes (COCs) were vitrified with Cryotop and then evaluated for fertility through in vitro fertilization (IVF). Although sperm-penetrated oocytes were observed to some extent (30-40%), the rate of pronuclear formation was low (9%) and none of them progressed to the two-cell stage. The results suggest that activation ability of cryopreserved oocytes was decreased by vitrification. We examined the localization and expression level of the type 1 inositol 1,4,5 trisphosphate receptor (IP3 R1), the channel responsible for Ca(2+) release during IVF in porcine oocytes. Localization of IP3 R1 close to the plasma membrane and total expression level of IP3 R1 protein were both decreased by vitrification. In conclusion, our present study indicates that vitrified-warmed porcine COCs showed a high survival rate but low fertility after IVF. This low fertility seems to be due to the decrease in IP3 R1 by the vitrification procedure.
Keywords: inositol trisphosphate receptor; oocyte; pig; vitrification
https://www.ncbi.nlm.nih.gov/pubmed/23607492
Inositol: effects on oocyte quality in patients undergoing ICSI. An open study.
Abstract:
Objectives: Nuclear and cytoplasmic competence of human oocyte is critical for future competence of the embryo upon which ultimately depends the outcome of an ART (Assisted Reproductive Technology) treatment. Follicular microenvironment in which the oocyte develops is crucial, and this must be taken into account particularly with the use of hormonal ovarian stimulation protocols. Inositol is an important element of the follicular environment and data support that its higher level in follicular fluid correlates with the development of a good oocyte. Aim of this study is to understand the effects of treatment with inositol on oocyte quality in a sample of patients undergoing ICSI (Intracytoplasmic Sperm Injection).
Patients and Methods: Assessment of oocyte/embryo quality and pregnancy rates in 149 patients divided, according to a controlled randomized pattern, into two groups: study group 1 treated with folic acid and inositol and control group 2 treated with folic acid alone.
Results: The number of patients with excellent and good oocyte quality appears to be significantly higher in group 1 (p = 0.02), as shown, they significantly increased the number of embryos of grade A transferred in the group 1 (p = 0.02) compared to group 2, despite being completely similar averages of total embryos transferred (total mean ± SD = 2.4 ± 0.8, group 1 mean ± SD = 2.4 ± 0.8, group 2 mean ± SD = 2.4 ± 0.8). There is not any significant difference between groups 1 and 2 in the number of positivity to β-hCG and in the number of biochemical pregnancies detected although it has a tendency to increase in the first and to decrease in the second for group 1. The increase in percentage of clinical pregnancies in group 1 was statistically significant (p = 0.02), whereas there was no apparent significance in the difference between the biochemical and clinical pregnancies in the two groups despite the positive trend in the study group.
Conclusions: Relying on "inositol help" to solidify our efforts, seems to be an easy path to help to deepen the effectiveness of its use in all patients still under 40 but with prior failed attempts at ICSI or diagnosed with PCOS or as "poor responders".
https://www.ncbi.nlm.nih.gov/pubmed/24302192
Follicular fluid and serum concentrations of myo-inositol in patients undergoing IVF: relationship with oocyte quality.
Chiu TT1, Rogers MS, Law EL, Briton-Jones CM, Cheung LP, Haines CJ.
Abstract:
Background: The follicular microenvironment is an important determinant of oocyte development. The aim of this study was to examine whether the myo-inositol (MI) content in human follicular fluid (FF) was associated with better oocyte quality.
Methods: A total of 53 patients treated with IVF was recruited to a prospective observational study. FF and serum samples collected were divided into two groups: group A consisted of FF associated with matured and fertilized oocytes, whilst group B was from follicles with immature and unfertilized oocytes.
Results: Patient's age, total ampoules of HMG used, days of stimulation, basal levels of FSH, estradiol (E(2)) levels on the day of HCG, and serum MI content were not significantly different between the two groups. FF volume and its MI content were significantly higher in group A compared with group B (P < 0.05). The levels of MI in FF were positively correlated with the amount of E(2) in their corresponding FF samples and also correlated with embryo quality.
Conclusions: We propose that higher concentrations of MI and E(2) in human FF appear to play a role in follicular maturity and provide a marker of good quality oocytes.
https://www.ncbi.nlm.nih.gov/pubmed/12042283
Effects of myo-inositol supplementation on oocyte's quality in PCOS patients: a double blind trial.
Ciotta L1, Stracquadanio M, Pagano I, Carbonaro A, Palumbo M, Gulino F.
Abstract:
Background: Polycystic ovary syndrome is the most common cause of chronic anovulation infertility in women in fertile period, and it's characterized by an increased production of androgens and estrogens. The administration of myo-inositol, a B complex vitamin, was associated with a decreased of serum testosterone and simultaneously, due to its ability to increase insulin sensitivity, women who received myo-inositol showed a great improvement of the ovulary function. Besides, the supplementation of inositol improves the oocytes' quality and increase the number of oocytes collected after ovarian stimulation in patients undergoing IVF (in vitro fertilization).
Aim: The aim of this study is to determine the effects of myo-inositol on oocyte's quality on a sample of women with polycystic ovary syndrome.
Material and Methods: The patients were divided into two groups: patients of Group A in-took 2 g of myo-inositol + 200 microg of folic acid (Inofolic, LO.LI. Pharma, Rome, Italy) while Group B only 200 microg of folic acid, both groups took the treatment twice a day, continuously for 3 months.
Results: At the end of treatment, the number of follicles of diameter > 15 mm, visible at ultrasound during stimulation, and the number of oocytes recovered at the time of pick-ups were found to be significantly greater in the group treated with myo-inositol, so as the aver-age number of embryos transferred and embryo Score S1. Significantly reduced was the average number of immature oocytes (vesicles germ and degenerated oocytes) too.
Conclusions: These data suggest that myo-inositol may be useful in the treatment of PCOS patients undergoing ovulation induction, both for its insulin-sensitizing activity, and its role in oocyte maturation.
https://www.ncbi.nlm.nih.gov/pubmed/21744744
Micronutrition and fertility problems in women: What is essential?
Article · April 2017 with 3 Reads
Abstract: New way of life of modern women (tobacco, alcohol, polluted environment, industrial food, endocrine disruptor, etc.) causes an increase of production of reactive oxygen species that affect female fertility. It was found that oxidative stress may damage the oocytes and may impair their fertilization capacity. The aim of this review of recent studies is to select natural ingredients able to reduce oxidative stress. A combination of vitamins (B, C and E), minerals (selenium, iodine) and myo-inositol could be useful as an alternative way, on top of balanced diet and lifestyle advice, for women planning to become pregnant including those with or without SOPK.
Micronutrition and fertility problems in women: What is essential?. Available from: https://www.researchgate.net/publication/319078771_Micronutrition_and_fertility_problems_in_women_What_is_essential?ev=publicSearchHeader&_sg=OLkflgbUBKR-DW8BnuhjARU6gATKsqVmAZziZwYqFsGhEAPbuv8Sktg1NM4DT_khpyLjwXNZ0JcnnAw
Could myo-inositol soft gel capsules outperform clomiphene in inducing ovulation? Results of a pilot study.
Rolland AL1, Peigné M, Plouvier P, Dumont A, Catteau-Jonard S, Dewailly D.
Abstract:
Objective: Insulin resistance is known to worsen polycystic ovarian syndrome (PCOS). The management of insulin resistance is crucial in the treatment of PCOS and insulin-sensitizing molecule as myo-inositol (MYO) seems to have promising effects. The aim of our pilot study was to study whether supplementation with MYO can improve patients' sensitivity to clomiphene citrate (CC) in terms of ovulation and pregnancy rates.
Patients and Methods: This study included 26 patients with PCOS, eligible to ovulation induction with CC. All of them received MYO in combination with CC and folic acid, following the usual protocol. Results concerning ovulation and pregnancy rates were compared to those from our historical cohort of PCOS patients treated with CC alone.
Results: Ovulation rate was significantly higher with MYO+CC than with CC alone (65.5% vs. 42%, p=0.0001). The number of patients sensitive to 50 mg/d was 54% with MYO vs. 40% in our reference cohort (NS). The total resistance rate was 19% vs. 27% in the reference cohort (NS). Cumulative pregnancy rate with MYO+CC was 53.8% vs. 42.2% with CC alone (NS). Pregnancy rates per initiated cycle were 16.1% with MYO vs. 12.6% in the historical cohort (NS).
Discussion: Although the differences were not significant for most outcomes, probably due to the small number of patients, our pilot study seemed to show a benefit of supplementation with MYO during ovulation induction with CC in PCOS patients.
Conclusions: This study proves the great interest of a RCT and re-opens the possibilities of insulin-sensitizing agents in the treatment of anovulatory patients with PCOS, such as natural products like MYO.
https://www.ncbi.nlm.nih.gov/pubmed/28724178
Antioxidants for female subfertility.
Showell MG1, Mackenzie-Proctor R, Jordan V, Hart RJ.
Abstract:
Background: A couple may be considered to have fertility problems if they have been trying to conceive for over a year with no success. This may affect up to a quarter of all couples planning a child. It is estimated that for 40% to 50% of couples, subfertility may result from factors affecting women. Antioxidants are thought to reduce the oxidative stress brought on by these conditions. Currently, limited evidence suggests that antioxidants improve fertility, and trials have explored this area with varied results. This review assesses the evidence for the effectiveness of different antioxidants in female subfertility.
Objectives: To determine whether supplementary oral antioxidants compared with placebo, no treatment/standard treatment or another antioxidant improve fertility outcomes for subfertile women.
Search Methods: We searched the following databases (from their inception to September 2016) with no language or date restriction: Cochrane Gynecology and Fertility Group (CGFG) specialized register, the Cochrane Central Register of Studies (CENTRAL CRSO), MEDLINE, Embase, PsycINFO, CINAHL and AMED. We checked reference lists of appropriate studies and searched for ongoing trials in the clinical trials registers.
Selectional Criteria: We included randomized controlled trials (RCTs) that compared any type, dose or combination of oral antioxidant supplement with placebo, no treatment or treatment with another antioxidant, among women attending a reproductive clinic. We excluded trials comparing antioxidants with fertility drugs alone and trials that only included fertile women attending a fertility clinic because of male partner infertility.
Data Collection and Analysis: Two review authors independently selected eligible studies, extracted the data and assessed the risk of bias of the included studies. The primary review outcome was live birth; secondary outcomes included clinical pregnancy rates and adverse events. We pooled studies using a fixed-effect model, and calculated odds ratios (ORs) with 95% confidence intervals (CIs) for the dichotomous outcomes of live birth, clinical pregnancy and adverse events. We assessed the overall quality of the evidence by applying GRADE criteria.
Main Results: We included 50 trials involving 6510 women. Investigators compared oral antioxidants, including combinations of antioxidants, N-acetyl-cysteine, melatonin, L-arginine, myo-inositol, D-chiro-inositol, carnitine, selenium, vitamin E, vitamin B complex, vitamin C, vitamin D+calcium, CoQ10, pentoxifylline and omega-3-polyunsaturated fatty acids versus placebo, no treatment/standard treatment or another antioxidant.Very low-quality evidence suggests that antioxidants may be associated with an increased live birth rate compared with placebo or no treatment/standard treatment (OR 2.13, 95% CI 1.45 to 3.12, P > 0.001, 8 RCTs, 651 women, I2 = 47%). This suggests that among subfertile women with an expected live birth rate of 20%, the rate among women using antioxidants would be between 26% and 43%.Very low-quality evidence suggests that antioxidants may be associated with an increased clinical pregnancy rate compared with placebo or no treatment/standard treatment (OR 1.52, 95% CI 1.31 to 1.76, P < 0.001, 26 RCTs, 4271 women, I2 = 66%). This suggests that among subfertile women with an expected clinical pregnancy rate of 22%, the rate among women using antioxidants would be between 27% and 33%. Heterogeneity was moderately high.There was insufficient evidence to determine whether there was a difference between the groups in rates of miscarriage (OR 0.79, 95% CI 0.58 to 1.08, P = 0.14, 18 RCTs, 2834 women, I2 = 23%, very low quality evidence). This suggests that, among subfertile women with an expected miscarriage rate of 7%, use of antioxidants would be expected to result in a miscarriage rate of between 4% and 7%. There was also insufficient evidence to determine whether there was a difference between the groups in rates of multiple pregnancy (OR 1.00, 95% CI 0.73 to 1.38, P = 0.98, 8 RCTs, 2163 women, I2 = 4%, very low quality evidence). This suggests that among subfertile women with an expected multiple pregnancy rate of 8%, use of antioxidants would be expected to result in a multiple pregnancy rate between 6% and 11%. Likewise, there was insufficient evidence to determine whether there was a difference between the groups in rates of gastrointestinal disturbances (OR 1.55, 95% CI 0.47 to 5.10, P = 0.47, 3 RCTs, 343 women, I2 = 0%, very low quality evidence). This suggests that among subfertile women with an expected gastrointestinal disturbance rate of 2%, use of antioxidants would be expected to result in a rate between 1% and 11%. Overall adverse events were reported by 35 trials in the meta-analysis, but there was insufficient evidence to draw any conclusions.Only one trial reported on live birth, clinical pregnancy or adverse effects in the antioxidant versus antioxidant comparison, and no conclusions could be drawn.Very low-quality evidence suggests that pentoxifylline may be associated with an increased clinical pregnancy rate compared with placebo or no treatment (OR 2.07, 95% CI 1.20 to 3.56, P = 0.009, 3 RCTs, 276 women, I2 = 0%). This suggests that among subfertile women with an expected clinical pregnancy rate of 25%, the rate among women using pentoxifylline would be between 28% and 53%.There was insufficient evidence to determine whether there was a difference between the groups in rates of miscarriage (OR 1.34, 95% CI 0.46 to 3.90, P = 0.58, 3 RCTs, 276 women, I2 = 0%) or multiple pregnancy (OR 0.78, 95% CI 0.20 to 3.09, one RCT, 112 women, very low quality evidence). This suggests that among subfertile women with an expected miscarriage rate of 4%, the rate among women using pentoxifylline would be between 2% and 15%. For multiple pregnancy, the data suggest that among subfertile women with an expected multiple pregnancy rate of 9%, the rate among women using pentoxifylline would be between 2% and 23%.The overall quality of evidence was limited by serious risk of bias associated with poor reporting of methods, imprecision and inconsistency.
Author's Conclusions: In this review, there was very low-quality evidence to show that taking an antioxidant may provide benefit for subfertile women, but insufficient evidence to draw any conclusions about adverse events. At this time, there is limited evidence in support of supplemental oral antioxidants for subfertile women.
Fertilichron male Research:
Iodine supplementation restores fertility of sheep exposed to iodine deficiency.
Ferri N1, Ulisse S, Aghini-Lombardi F, Graziano FM, Di Mattia T, Russo FP, Arizzi M, Baldini E, Trimboli P, Attanasio D, Fumarola A, Pinchera A, D'Armiento M.
Abstract: The aims of the study were to monitor sheep iodine intake in different sheep breeding farms in Abruzzo and to evaluate the effects of iodinesupplementation on ovine fertility. The urinary iodine concentrations (UIC) in animals of 8 out of the 11 breeding farms analyzed were borderline (UIC 100-150 microg/l) or very low (UIC < or = 50 microg/l). Only animals bred in 3 farms showed an adequate iodine intake with a mean UIC > or = 300 microg/l. Animals with very low iodine intake had lower T4 and T3 (p < 0.01) serum levels, compared to those with adequate iodine intake. To investigate the effects of iodine supplementation on ovine fertility, 32 ewes and 20 rams, characterized by low UIC, were randomly divided into 2 groups. One group (16 ewes and 10 rams) received a sc injection of 1 ml of Lipiodol, containing 480 mg of iodine, while the remaining animals were employed as control. This treatment was able to maintain UIC above 300 microg/l for 3 months and to increase T4 and T3 serum levels (p < 0.01). After 9 months, the fertility of control and treated animals was assessed by monitoring the rate of successful matings by ultrasonography. The results showed that 100% of treated ewes mated with treated rams were pregnant vs 37% of the control ewes mated with control rams (p = 0.007). The iodine content was 4-fold higher in milk from treated ewes (2393 +/- 453 microg/l), compared to controls (675 +/- 154 microg/l). The results demonstrated that iodine supplementation restores fertility of sheep living in iodinedeficient areas and may represent a means to achieve a silent iodine prophylaxis of local populations.
https://www.ncbi.nlm.nih.gov/pubmed/15008245
Fertilichron female Research:
Micronutrition and fertility problems in women: What is essential?
Article · April 2017 with 3 Reads
Abstract: New way of life of modern women (tobacco, alcohol, polluted environment, industrial food, endocrine disruptor, etc.) causes an increase of production of reactive oxygen species that affect female fertility. It was found that oxidative stress may damage the oocytes and may impair their fertilization capacity. The aim of this review of recent studies is to select natural ingredients able to reduce oxidative stress. A combination of vitamins (B, C and E), minerals (selenium, iodine) and myo-inositol could be useful as an alternative way, on top of balanced diet and lifestyle advice, for women planning to become pregnant including those with or without SOPK.
Micronutrition and fertility problems in women: What is essential?. Available from: https://www.researchgate.net/publication/319078771_Micronutrition_and_fertility_problems_in_women_What_is_essential?ev=publicSearchHeader&_sg=OLkflgbUBKR-DW8BnuhjARU6gATKsqVmAZziZwYqFsGhEAPbuv8Sktg1NM4DT_khpyLjwXNZ0JcnnAw
The effect of micronutrient supplements on female fertility.
Abstract:
Purpose of Review: Benefit of micronutrient supplementation on female fertility.
Recent Findings: Reports of randomized trials are rare. Most studies are focused on multivitamin supplementations. For some micronutrients, a positive impact on fertility could be shown. This article reviews the available clinical studies as well as the pathophysiological background of possible effects and summarizes the potential benefits of selected micronutrients on female fertility.
Summary: Apart from lowering the malformation risk by periconceptional supplementation of folic acid, substitution with different micronutrients, particularly folic acid, vitamin B6, vitamin C, vitamin D, vitamin E, iodine, selenium, iron, and DHA might have a positive impact on infertility treatment. The multivitamin formulation should take the pathophysiology, clinical studies, and upper limits into account.
https://www.ncbi.nlm.nih.gov/pubmed/23571830
Iodine supplementation restores fertility of sheep exposed to iodine deficiency.
Ferri N1, Ulisse S, Aghini-Lombardi F, Graziano FM, Di Mattia T, Russo FP, Arizzi M, Baldini E, Trimboli P, Attanasio D, Fumarola A, Pinchera A, D'Armiento M.
Abstract: The aims of the study were to monitor sheep iodine intake in different sheep breeding farms in Abruzzo and to evaluate the effects of iodinesupplementation on ovine fertility. The urinary iodine concentrations (UIC) in animals of 8 out of the 11 breeding farms analyzed were borderline (UIC 100-150 microg/l) or very low (UIC < or = 50 microg/l). Only animals bred in 3 farms showed an adequate iodine intake with a mean UIC > or = 300 microg/l. Animals with very low iodine intake had lower T4 and T3 (p < 0.01) serum levels, compared to those with adequate iodine intake. To investigate the effects of iodine supplementation on ovine fertility, 32 ewes and 20 rams, characterized by low UIC, were randomly divided into 2 groups. One group (16 ewes and 10 rams) received a sc injection of 1 ml of Lipiodol, containing 480 mg of iodine, while the remaining animals were employed as control. This treatment was able to maintain UIC above 300 microg/l for 3 months and to increase T4 and T3 serum levels (p < 0.01). After 9 months, the fertility of control and treated animals was assessed by monitoring the rate of successful matings by ultrasonography. The results showed that 100% of treated ewes mated with treated rams were pregnant vs 37% of the control ewes mated with control rams (p = 0.007). The iodine content was 4-fold higher in milk from treated ewes (2393 +/- 453 microg/l), compared to controls (675 +/- 154 microg/l). The results demonstrated that iodine supplementation restores fertility of sheep living in iodinedeficient areas and may represent a means to achieve a silent iodine prophylaxis of local populations.
Fertilichron male Research:
The role of arginine, indomethacin and kallikrein in the treatment of oligoasthenospermia
(n=45, double blind, paralell group study for 3 month).
Aydin Set al; Int Urol Nephrol 1995
We have treated 45 patients with various degrees of oligospermia and asthenospermia with arginine, indomethacin and kallikrein. Fifteen patients have received the amino acid L-arginine hydrochloride, 15 the antiinflammatory agent indomethacin, while 15 others the enzyme kallikrein. These drugs have been administered for at least 3 months to encompass a complete cycle of spermatogenesis.
As a result, treatment with these drugs has increased sperm count and motility to some extent. Three pregnancies (20%) have been obtained by arginine and one pregnancy (6.6%) by indomethacin. Though arginine offers some hope for the future, improvement of the fertilizing capacity with these drugs is still controversial.
https://rd.springer.com/article/10.1007%2FBF02551320
Lipovac M, Bodner F, Imhof M, Chedraui P.
Reprod Biol Endocrinol.2016 Dec 9;14(1):84.
Comparison of the effect of a combination of eight micronutrients versus a standard mono preparation on sperm parameters.
Abstract:
Background: There are reports showing that l-carnitine alone or in combination with other micronutrients improve sperm parameters. However, comparative studies are still lacking. This study was carried out to compare the short term effects of a combination of eight micronutrients including l-carnitine vs. a mono-substance (l-carnitine alone) on sperm parameters.
Methods: This was a prospective, open-labelled, nonrandomized study that included male subjects (20 to 60 years) with at least 1 year of subfertility and at least one pathological semen analysis who received 3 months treatment with a mono-substance (500 mg l-carnitine/twice a day, n = 156) or a combined compound (440 mg l-carnitine + 250 mg l-arginine + 40 mg zinc + 120 mg vitamin E + 80 mg glutathione + 60 μg selenium + 15 mg coenzyme Q10 + 800 μg folic acid/once a day, n = 143) for the same time period. Sperm parameters were analyzed before and after treatment and groups comparisons performed.
Results: Baseline characteristics were similar among studied groups (age and body mass indices). Semen parameters (volume, density, overall progressive motility [including slow and fast motility]) and percentage of sperm with normal morphology improved after 3 months in both groups as compared to baseline. However, relative change (expressed as % increase of absolute values) for sperm density and overall progressive motility (including fast motility) was found to be higher for the combined micronutrient treatment group as compared to the mono-treatment using l-carnitine alone.
Conclusion: Both analyzed groups displayed a positive short term effect on all sperm parameters; however effect on density and motility was significantly better for the combined formulation. There is need for more research in this matter that includes long term outcome data.
Fertilichron female Research:
Negative association of L-arginine methylation products with oocyte numbers.
Bódis J1, Várnagy A, Sulyok E, Kovács GL, Martens-Lobenhoffer J, Bode-Böger SM.
Abstract:
Backgrounds: The aim of this study was to determine the concentrations of L-arginine and methylarginines in follicular fluid obtained from women participating in our IVF program and to find clinical correlates of these biochemical parameters.
Methods: Follicular fluid was obtained from 108 women by ultrasonography guided transvaginal puncture following controlled ovarian hyperstimulation. Follicular fluid L-arginine, asymmetric dimethylarginine (ADMA), symmetric dimethylarginine (SDMA) and monomethylarginine (MMA) concentrations were determined with liquid chromatography-tandem mass spectrometry. The integrated index of arginine methylation (arg-MI) was calculated according to the formula: arg-MI = (ADMA + SDMA)/MMA.
Results: There were significant inverse relationships between IVF embryo number and follicular fluid L-arginine (r = -0.507, P < 0.001), ADMA (r = -0.356, P < 0.024), SDMA (r = -0.347, P < 0.028), MMA (r = -0.449, P < 0.004) and to L-arginine/ADMA ratio (r = -0.328, P < 0.031). By contrast, arg-MI was directly related to IVF embryo number (r = 0.426, P < 0.006). Moreover, the number of IVF oocytes was also inversely related to ADMA (r = -0.202, P < 0.037) and MMA (r = -0.384, P < 0.012) and positively to arg-MI (r = 0.450, P < 0.03).
Conclusions: The elevated levels of follicular fluid l-arginine and methylarginines appear to have an adverse influence on the reproductive processes as reflected by a reduction in the number of oocytes and embryos conceived. In contrast, the integrated methylation index proved to be positively correlated to the above parameters of fertilization.
https://www.ncbi.nlm.nih.gov/pubmed/20870683
Antioxidants for female subfertility.
Showell MG1, Mackenzie-Proctor R, Jordan V, Hart RJ.
Abstract:
Background: A couple may be considered to have fertility problems if they have been trying to conceive for over a year with no success. This may affect up to a quarter of all couples planning a child. It is estimated that for 40% to 50% of couples, subfertility may result from factors affecting women. Antioxidants are thought to reduce the oxidative stress brought on by these conditions. Currently, limited evidence suggests that antioxidants improve fertility, and trials have explored this area with varied results. This review assesses the evidence for the effectiveness of different antioxidants in female subfertility.
Objectives: To determine whether supplementary oral antioxidants compared with placebo, no treatment/standard treatment or another antioxidant improve fertility outcomes for subfertile women.
Search Methods: We searched the following databases (from their inception to September 2016) with no language or date restriction: Cochrane Gynecology and Fertility Group (CGFG) specialized register, the Cochrane Central Register of Studies (CENTRAL CRSO), MEDLINE, Embase, PsycINFO, CINAHL and AMED. We checked reference lists of appropriate studies and searched for ongoing trials in the clinical trials registers.
Selection Criteria: We included randomized controlled trials (RCTs) that compared any type, dose or combination of oral antioxidant supplement with placebo, no treatment or treatment with another antioxidant, among women attending a reproductive clinic. We excluded trials comparing antioxidants with fertility drugs alone and trials that only included fertile women attending a fertility clinic because of male partner infertility.
Data Collection and Analysis: Two review authors independently selected eligible studies, extracted the data and assessed the risk of bias of the included studies. The primary review outcome was live birth; secondary outcomes included clinical pregnancy rates and adverse events. We pooled studies using a fixed-effect model, and calculated odds ratios (ORs) with 95% confidence intervals (CIs) for the dichotomous outcomes of live birth, clinical pregnancy and adverse events. We assessed the overall quality of the evidence by applying GRADE criteria.
Main Results: We included 50 trials involving 6510 women. Investigators compared oral antioxidants, including combinations of antioxidants, N-acetyl-cysteine, melatonin, L-arginine, myo-inositol, D-chiro-inositol, carnitine, selenium, vitamin E, vitamin B complex, vitamin C, vitamin D+calcium, CoQ10, pentoxifylline and omega-3-polyunsaturated fatty acids versus placebo, no treatment/standard treatment or another antioxidant.Very low-quality evidence suggests that antioxidants may be associated with an increased live birth rate compared with placebo or no treatment/standard treatment (OR 2.13, 95% CI 1.45 to 3.12, P > 0.001, 8 RCTs, 651 women, I2 = 47%). This suggests that among subfertile women with an expected live birth rate of 20%, the rate among women using antioxidants would be between 26% and 43%.Very low-quality evidence suggests that antioxidants may be associated with an increased clinical pregnancy rate compared with placebo or no treatment/standard treatment (OR 1.52, 95% CI 1.31 to 1.76, P < 0.001, 26 RCTs, 4271 women, I2 = 66%). This suggests that among subfertile women with an expected clinical pregnancy rate of 22%, the rate among women using antioxidants would be between 27% and 33%. Heterogeneity was moderately high.There was insufficient evidence to determine whether there was a difference between the groups in rates of miscarriage (OR 0.79, 95% CI 0.58 to 1.08, P = 0.14, 18 RCTs, 2834 women, I2 = 23%, very low quality evidence). This suggests that, among subfertile women with an expected miscarriage rate of 7%, use of antioxidants would be expected to result in a miscarriage rate of between 4% and 7%. There was also insufficient evidence to determine whether there was a difference between the groups in rates of multiple pregnancy (OR 1.00, 95% CI 0.73 to 1.38, P = 0.98, 8 RCTs, 2163 women, I2 = 4%, very low quality evidence). This suggests that among subfertile women with an expected multiple pregnancy rate of 8%, use of antioxidants would be expected to result in a multiple pregnancy rate between 6% and 11%. Likewise, there was insufficient evidence to determine whether there was a difference between the groups in rates of gastrointestinal disturbances (OR 1.55, 95% CI 0.47 to 5.10, P = 0.47, 3 RCTs, 343 women, I2 = 0%, very low quality evidence). This suggests that among subfertile women with an expected gastrointestinal disturbance rate of 2%, use of antioxidants would be expected to result in a rate between 1% and 11%. Overall adverse events were reported by 35 trials in the meta-analysis, but there was insufficient evidence to draw any conclusions.Only one trial reported on live birth, clinical pregnancy or adverse effects in the antioxidant versus antioxidant comparison, and no conclusions could be drawn.Very low-quality evidence suggests that pentoxifylline may be associated with an increased clinical pregnancy rate compared with placebo or no treatment (OR 2.07, 95% CI 1.20 to 3.56, P = 0.009, 3 RCTs, 276 women, I2 = 0%). This suggests that among subfertile women with an expected clinical pregnancy rate of 25%, the rate among women using pentoxifylline would be between 28% and 53%.There was insufficient evidence to determine whether there was a difference between the groups in rates of miscarriage (OR 1.34, 95% CI 0.46 to 3.90, P = 0.58, 3 RCTs, 276 women, I2 = 0%) or multiple pregnancy (OR 0.78, 95% CI 0.20 to 3.09, one RCT, 112 women, very low quality evidence). This suggests that among subfertile women with an expected miscarriage rate of 4%, the rate among women using pentoxifylline would be between 2% and 15%. For multiple pregnancy, the data suggest that among subfertile women with an expected multiple pregnancy rate of 9%, the rate among women using pentoxifylline would be between 2% and 23%.The overall quality of evidence was limited by serious risk of bias associated with poor reporting of methods, imprecision and inconsistency.
Authors' Conclusions: In this review, there was very low-quality evidence to show that taking an antioxidant may provide benefit for subfertile women, but insufficient evidence to draw any conclusions about adverse events. At this time, there is limited evidence in support of supplemental oral antioxidants for subfertile women.
Fertilichron male Research:
Human sperm DNA oxidation, motility and viability in the presence of l-carnitine during in vitro incubation and centrifugation
(n=55 fertile, experimental study).
Banihani Set al; Andrologia 2011
Abstract: In vitro incubation and centrifugation is known to decrease human sperm quality. In the human body, besides its antioxidant effects, L-carnitine (LC) facilitates the transport of activated fatty acids from the cytosol to the mitochondrial matrix. In this study, we investigated the effect of LC on human sperm motility, viability and DNA oxidation after incubation and centrifugation, following the sperm preparation protocols of assisted reproduction. Normozoospermic semen samples (n = 55) were analysed according to the World Health Organization (WHO) guidelines. LC concentrations that are not toxic to spermatozoa as determined by sperm motility and viability were standardised after 2 and 4 h of incubation at 37 °C. Semen samples to which the optimal LC concentrations were added were also centrifuged for 20 min at 300 g and analysed for sperm motility, viability and DNA oxidation. Sperm motility was improved at 0.5 mg ml(-1) LC after incubation and centrifugation with 5 × 10(6) sperm ml(-1). Higher concentration of LC (50 mg ml(-1)) significantly decreased sperm motility and viability. LC did not alter the baseline of sperm DNA oxidation during both incubation and centrifugation. In conclusion, LC may enhance sperm motility following incubation and centrifugation, while it might not affect sperm viability and DNA oxidation.
Human sperm DNA oxidation, motility and viability in the presence of L-carnitine during in vitro incubation and centrifugation | Request PDF. Available from: https://www.researchgate.net/publication/51676563_Human_sperm_DNA_oxidation_motility_and_viability_in_the_presence_of_L-carnitine_during_in_vitro_incubation_and_centrifugation
Level of free L-carnitine in human seminal plasma and its correlation with semen quality
(n= normozoospermia, n=117, oligozoospermia, n=81, azoospermia, n=32, epidemiological study).
Li Ket al; Zhonghua Nan Ke Xue 2007
Abstract: To evaluate the difference of the free L-carnitine level in seminal plasma between fertile and infertile men and the correlation of free L-carnitine with semen quality, and to study the effect of L-carnitine on male fertility and its role in the evaluation and treatment of male infertility. Semen samples of 230 infertile (normozoospermia, n=117, oligozoospermia, n=81, azoospermia, n=32) and 30 fertile men were collected and the level of free L-carnitine in seminal plasma and such sperm parameters as sperm concentration, motility and vitality, were determined by high performance liquid chromatography and computer-assisted semen analysis system, respectively. The results were analyzed with the SPSS 12.0 software. The level of free L-carnitine in the seminal plasma of the fertile men was significantly higher than that of the infertile (P < 0.01). The lower the sperm concentration, the weaker the sperm vitality, the more significant the difference. The level of free L-carnitine in the semen was positively correlated with sperm concentration (r = 0.521, P < 0.001), and sperm motility (r = 0.319, P < 0.001) and vitality (r = 0.251, P < 0.001). The level of free L-carnitine in seminal plasma, significantly correlated with sperm concentration, motility and vitality, can be taken as a biochemical index used as a guidance for the clinical treatment of male infertility as well as for the study on the mechanisms of male reproduction.
[Level of free L-carnitine in human seminal plasma and its correlation with semen quality]. Available from: https://www.researchgate.net/publication/6460687_Level_of_free_L-carnitine_in_human_seminal_plasma_and_its_correlation_with_semen_quality
Effect of L-carnitine and/or L-acetyl-carnitine in nutrition treatment for male infertility: a systematic review
(meta-analysis).
Zhou Xet al; Asia Pac J Clin Nutr 2007
Abstract: The aim of this systematic review was to quantify the efficacy of L-carnitine (LC) and/or L-acetyl-carnitine (LAC) in nutrition treatment for male infertility according to present clinical evidence. Biomedical databases were searched to collect related clinical trials and nine relevant randomized controlled trials (RCTs) were included. The quality of the RCTs was assessed based on their performance in randomization, blinding, and allocation concealment. The meta-analysis compared LC and /or LAC therapy to placebo treatment found significant improvement in pregnancy rate (OR = 4.10, 95% CI (2.08, 8.08), p< 0.0001), total sperm motility (WMD = 7.43, 95% CI (1.72, 13.14), p = 0.04, forward sperm motility (WMD = 11.83, 95% CI (0.49, 23.16), p = 0.04) and atypical sperm cell (WMD = -5.72, 95% CI (-7.89, -3.56), p< 0.00001). However, no significant difference was found in the sperm concentration (WMD = 5.69, 95% CI (-4.47, 15.84), p = 0.27) and semen volume (WMD = 0.28, 95% CI (-0.02, 0.58), p = 0.07). In conclusion, the administration of LC and/or LAC may be effective in improving pregnancy rate and sperm kinetic features in patients affected by male infertility. However, the exact efficacy of carnitines on male infertility needs to be confirmed by further investigations.
Effects of L-carnitine on Infertile Men’s Spermogram; a Randomized Clinical Trial
Volume 10, Issue 4, Number 41 / January-March 2010
(pages 245-251)
Introduction: Male infertility is one of the most challenging problems in andrology. The common cause of male infertility is related to disorders in sperm production and its improvement is synonymous with better treatment outcomes. Although, the etiology of infertility is not clear in most cases but different treatment options have been suggested to increase sperm count and motility. L-carnitine, which is found in different food items and it is derived from lysine and methionine, is a substance essential for the oxidation of long-chain fatty acids in the mitochondria and protection of cell membranes from damages caused by free oxygen radicals. This study was done to evaluate the efficacy of L-carnitine in improving sperm quality in infertile men.Materials and Methods: This double blind randomized cross-over, clinical trial was conducted on 30 infertile men attending Sari Imam Khomeini Hospital’s Infertility Clinic during 2005- 2006. Subjects that had at least two abnormal spermograms, based on WHO criteria, with a two-week interval during four weeks and their gonadotropins, testosterone an prolactin concentrations were within normal range were recruited for the study. The exclusion criteria were composed of individuals with medical conditions other than infertility such as grade 3 or 4 varicocele, testicular atrophy, ejaculatory disorders, use of any medications in the past two months prior to the study, azoospermia, endocrinological disorders, ICSI candidacy for severe spermogram abnormalities or other causes of infertility.The patients were randomly allocated to two groups of A and B. Group A and B received L-carnitine and placebo 2g/day for 8 weeks respectively. After a washout period of 8 weeks, the two groups, changed place and received placebo and L-carnitine (2g/day×8w). Sperm analyses were done in four stages: Before and after the first intervention, at the end of washout period and after the second intervention.Results: There were significant improvements in mean sperm concentration and progressive sperm motility upon two months of L-carnitine intake (p<0.05) but no significant changes were found in sperm volume or morphology. The aforementioned changes retracted to the primary status after two months. No changes were seen following the intake of placebos in the cases.Conclusion: L-carnitine intake effectively improved the mean sperm count and progressive sperm motility. However, confirmation of these results warrants more thorough clinical trials.
Antioxidants and Phytocompounds on Seminal Oxidative Stress
Article (PDF Available) · March 2017 with 184 Reads
DOI: 10.3390/diseases5010009
Abstract: Defective sperm function has been identified as the most common cause of infertility. The objective of this study was to review recent findings on the effects of various antioxidants on male fertility. High amounts of poly unsaturated fatty acid are found in the mammalian spermatozoa membranes, thereby making them susceptible to lipid peroxidation. Although, free radicals and reactive oxygen species (ROS) play major roles in reproduction, they are strongly associated with oxidative stress. Furthermore, factors such as obesity, inflammation, pollutants and cigarette smoking are negatively correlated with spermatogenesis. Endogenous antioxidants system exists to mediate these damages. In a normal physiological state, the seminal plasma contains antioxidant enzyme mechanism that is capable of quenching these ROS as well as protecting the spermatozoa against any likely damage. However, high level of ROS triggered by inflammatory cells and oxidation of fatty acid in obese subjects may down play antioxidant mechanism resulting in oxidative stress. Evaluation of such oxidative stress is the first step in the treatment of male infertility through administration of suitable antioxidant. Notably, antioxidant such as vitamin E and C, carotenoids and carnitine have been found beneficial in restoring a balance between ROS generation and scavenging activities. There are emerging evidences that herbal products can also boost male reproductive functions. Nonetheless, a good lifestyle, regular exercise, avoidance of stress and observing safety rules at work are habits that can reverse male infertility.
Discover the world's research
(PDF) Male Infertility: The Effect of Natural Antioxidants and Phytocompounds on Seminal Oxidative Stress. Available from: https://www.researchgate.net/publication/314202739_Male_Infertility_The_Effect_of_Natural_Antioxidants_and_Phytocompounds_on_Seminal_Oxidative_Stress
Lipovac M, Bodner F, Imhof M, Chedraui P.
Reprod Biol Endocrinol.2016 Dec 9;14(1):84.
Comparison of the effect of a combination of eight micronutrients versus a standard mono preparation on sperm parameters.
Abstract:
Background: There are reports showing that l-carnitine alone or in combination with other micronutrients improve sperm parameters. However, comparative studies are still lacking. This study was carried out to compare the short term effects of a combination of eight micronutrients including l-carnitine vs. a mono-substance (l-carnitine alone) on sperm parameters.
Methods: This was a prospective, open-labelled, nonrandomized study that included male subjects (20 to 60 years) with at least 1 year of subfertility and at least one pathological semen analysis who received 3 months treatment with a mono-substance (500 mg l-carnitine/twice a day, n = 156) or a combined compound (440 mg l-carnitine + 250 mg l-arginine + 40 mg zinc + 120 mg vitamin E + 80 mg glutathione + 60 μg selenium + 15 mg coenzyme Q10 + 800 μg folic acid/once a day, n = 143) for the same time period. Sperm parameters were analyzed before and after treatment and groups comparisons performed.
Results: Baseline characteristics were similar among studied groups (age and body mass indices). Semen parameters (volume, density, overall progressive motility [including slow and fast motility]) and percentage of sperm with normal morphology improved after 3 months in both groups as compared to baseline. However, relative change (expressed as % increase of absolute values) for sperm density and overall progressive motility (including fast motility) was found to be higher for the combined micronutrient treatment group as compared to the mono-treatment using l-carnitine alone.
Conclusion: Both analyzed groups displayed a positive short term effect on all sperm parameters; however effect on density and motility was significantly better for the combined formulation. There is need for more research in this matter that includes long term outcome data.
Sofimajidpour H, Ghaderi E, Ganji O.
J Clin Diagn Res.2016 Apr;10(4):PC07-10. doi: 10.7860/JCDR/2016/18464.7557. Epub 2016 Apr 1.
Comparison of the Effects of Varicocelectomy and Oral L-carnitine on Sperm Parameters in Infertile Men with Varicocele.
Abstract:
Background: Varicocele is defined as dilated and twisted veins of the pampiniform plexus in the spermatic cord. It is the most common cause of male infertility. There are various medical and surgical procedures for the treatment of this disease.
Aim: This study was aimed to compare the effects of oral administration of L-Carnitine and varicocelectomy on spermogram parameters.
Materials and Methods: This study was conducted as a double blind clinical trial without randomization. Inclusion criteria were, all married infertile men with varicocele. Patients chose their treatment personally and spermogram was carried out for all patients before and after the third and sixth months of treatment. Then, the sperm parameters of the two groups were compared using repeated measures ANOVA.
Results: In our study, trend of sperm count in the surgery group changed from 22 to 28.61 million (vs 34.6 to 45.37 in L-Carnitine group), motility changed from 21.74 to 35.38 percent (vs 33.9 to 47.48 in L-Carnitine group), normal sperm morphology changed from 46.25 to 60 percent (vs 56.61 to 69.7 in L-Carnitine group) and volume of semen changed from 3.5 to 4.17 cc (vs 2.95 to 4.33 in L-Carnitine group). These values were not statistically different between the two groups.
Conclusion: Based on the results of this study, we can say that medicinal treatment by administration of oral L-Carnitine is as effective as varicocelectomy in improving semen parameters and can be used as an alternative to surgery for varicocele grade II.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4866177/
Balercia G, Regoli F, Armeni T, Koverech A, Mantero F, Boscaro M.
Fertil Steril.2005 Sep;84(3):662-71.
Placebo-controlled double-blind randomized trial on the use of L-carnitine, L-acetylcarnitine, or combined L-carnitine and L-acetylcarnitine in men with idiopathic asthenozoospermia.
Abstract:
Objective: To evaluate the effectiveness of L-carnitine (LC) or L-acetyl-carnitine (LAC) or combined LC and LAC treatment in improving semen kinetic parameters and the total oxyradical scavenging capacity in semen.
Design: Placebo-controlled, double-blind, randomized trial.
Setting: Andrology unit, Department of Internal Medicine, Polytechnic University of Marche, Italy.
Patients: Sixty infertile men, ages 20 to 40 years, with the following baseline sperm selection criteria: concentration > 20 x 10(6)/mL, sperm forward motility < 50%, and normal sperm morphology > 30%; 59 patients completed the study.
Interventions: Patients underwent a double-blind therapy of LC 3 g/d, LAC 3 g/d, a combination of LC 2 g/d and LAC 1 g/d, or placebo. The study design was 1 month of run in, 6 months of therapy or placebo, and 3 months of follow-up evaluation.
Main Outcome Measures: Variations in semen parameters used for patient selection, and variations in total oxyradical scavenging capacity of the seminal fluid.
Results: Sperm cell motility (total and forward, including kinetic features determined by computer-assisted sperm analysis) increased in patients to whom LAC was administered both alone or in combination with LC; combined LC + LAC therapy led to a significant improvement of straight progressive velocity after 3 months. The total oxyradical scavenging capacity of the semen toward hydroxyl and peroxyl radicals also increased and was positively correlated with the improvement of kinetic features. Patients with lower baseline values of motility and total oxyradical scavenging capacity of the seminal fluid had a significantly higher probability of responding to the treatment.
Conclusions: The administration of LC and LAC is effective in increasing sperm kinetic features in patients affected by idiopathic asthenozoospemia and improves the total oxyradical scavenging capacity of the seminal fluid in the same population.
https://www.ncbi.nlm.nih.gov/pubmed/16169400
Lenzi A, Sgrò P, Salacone P, Paoli D, Gilio B, Lombardo F, Santulli M, Agarwal A, Gandini L.
Fertil Steril.2004 Jun;81(6):1578-84.
A placebo-controlled double-blind randomized trial of the use of combined l-carnitine and l-acetyl-carnitine treatment in men with asthenozoospermia.
Abstract:
Objective: To determine the efficacy of combined l-carnitine and l-acetyl-carnitine therapy in infertile males with oligo-astheno-teratozoospermia.
Design: Placebo-controlled double-blind randomized trial.
Setting: University tertiary referral center.
Patients: Sixty infertile patients (aged 20-40 years) with the following baseline sperm selection criteria: concentration, 10 to 40 x 10(6)/mL; forward motility, <15%; total motility, 10% to 40%; and atypical forms, <80%. Fifty-six patients completed the study.
Intervention: Patients were submitted to a combined treatment of l-carnitine (2 g/d) and l-acetyl-carnitine (1 g/d) or of placebo; the study design was 2 months' wash-out, 6 months of therapy or of placebo, and 2 months' follow-up.
Main Outcome Measures: Variation in the semen parameters that were used for patient selection.
Results: Even though increases were seen in all sperm parameters after combined carnitine treatment, the most significant improvement in sperm motility (both forward and total) was present in patients who had lower initial absolute values of motile sperm (<4 x 10(6) forward or <5 x 10(6) total motile spermatozoa per ejaculate).
Conclusions: Combined treatment with l-carnitine and l-acetyl-carnitine in a controlled study of efficacy was effective in increasing sperm motility, especially in groups with lower baseline levels.
Fertilichron male Research:
Male Infertility: The Effect of Natural Antioxidants and Phytocompounds on Seminal Oxidative Stress.
Adewoyin M1, Ibrahim M2, Roszaman R3, Isa MLM4, Alewi NAM5, Rafa AAA6, Anuar MNN1.
Abstract: Defective sperm function has been identified as the most common cause of infertility. The objective of this study was to review recent findings on the effects of various antioxidants on male fertility. High amounts of poly unsaturated fatty acid are found in the mammalian spermatozoamembranes, thereby making them susceptible to lipid peroxidation. Although, free radicals and reactive oxygen species (ROS) play major roles in reproduction, they are strongly associated with oxidative stress. Furthermore, factors such as obesity, inflammation, pollutants and cigarette smoking are negatively correlated with spermatogenesis. Endogenous antioxidants system exists to mediate these damages. In a normal physiological state, the seminal plasma contains antioxidant enzyme mechanism that is capable of quenching these ROS as well as protecting the spermatozoa against any likely damage. However, high level of ROS triggered by inflammatory cells and oxidation of fatty acid in obese subjects may down play antioxidant mechanism resulting in oxidative stress. Evaluation of such oxidative stress is the first step in the treatment of male infertility through administration of suitable antioxidant. Notably, antioxidant such as vitamin E and C, carotenoids and carnitine have been found beneficial in restoring a balance between ROS generation and scavenging activities. There are emerging evidences that herbal products can also boost male reproductive functions. Nonetheless, a good lifestyle, regular exercise, avoidance of stress and observing safety rules at work are habits that can reverse male infertility.
Fertilichron male Research:
Lycopene therapy in idiopathic male infertility - a preliminary report.
(n=30, open trail per 3 month).
Gupta NPet al., Int Urol Nephrol 2002
Abstract: Excessive generation of reactive oxygen species (ROS) containing free oxygen radicals has been identified as one of the causes of male infertility. Lycopene is a component of human redox defence mechanism against free radicals. It is found in high concentrations in the testes and seminal plasma and decreased levels have been demonstrated in men suffering from infertility. We evaluated the effect of oral lycopene therapy in men with idiopathic infertility. Beginning March 2000, thirty men with idiopathic non-obstructive oligo/astheno/teratozoospermia were enrolled for the trial. All patients were administered 2000 mcg of Lycopene, twice a day for three months. Semen analysis was performed at three months and sperm concentration, motility and morphology were evaluated. All patients completed the trial without any complications. Twenty patients (66%) showed an improvement in sperm concentration, sixteen (53%) had improved motility and fourteen (46%) showed improvement in sperm morphology. In cases showing an improvement, the median change in concentration was 22 million/ml, motility 25% and morphology 10%. The improvement in concentration and motility were statistically significant. Baseline sperm concentration less than 5 million/ml was associated with no significant improvement. Higher baseline concentrations were associated with significant improvement and resulted in six pregnancies in 26 patients (23%). Oral Lycopene therapy seems to have a role in the management of idiopathic male infertility. Maximum improvement seems to occur in the sperm concentration (66% cases). Patients without severe oligospermia (sperm density > 5 million/ml) may be given a trial of therapy with lycopene. However, larger randomised controlled trials are essential before definitive therapeutic guidelines can be made.
(PDF) Lycopene therapy in idiopathic male.... Available from: https://www.researchgate.net/publication/10629931_Lycopene_therapy_in_idiopathic_male_infertility_-_A_preliminary_report
Lycopene, an antioxidant carotenoid, attenuates testicular injury caused by ischemia/reperfusion in rats.
Tohoku J Exp Med.2009 Jun;218(2):141-7.
Hekimoglu A, Kurcer Z, Aral F, Baba F, Sahna E, Atessahin A.
Abstract: Testicular torsion is a common syndrome that could lead to infertility. We investigated the therapeutic effects of lycopene, an antioxidant caretenoid, on testicular ischemia/reperfusion (IR) injury that resembles testicular torsion. Male Wistar albino rats were divided into three groups: sham (n = 6), IR (n = 18), and ischemia/reperfusion with lycopene (IRL, n = 18). Left testicular artery and vein was occluded for 1 h, followed by reperfusion of 3 h, 24 h or 30 days in IR and IRL animals. Either corn oil (vehicle) or lycopene (4 mg/kg) was administrated once daily by gavage to IR or IRL animals, respectively, 5 min after ischemia. Sham-operated animals were treated with vehicle by gavage 5 min after the operation. IR decreased sperm motility and concentration in both ipsilateral and contralateral testes and increased abnormal sperm rate in ipsilateral testis after 30 days of reperfusion. Treatment with lycopene increased the motility in bilateral testes and decreased the rate of abnormal sperm in ipsilateral testis to the sham level, but did not increase sperm concentration in bilateral testes. IR increased the activities of catalase and glutathione peroxidase and the level of reduced glutathione by 24 h of reperfusion, but malondialdehyde remained unchanged. Lycopene treatment restored the enzyme activities but not the reduced glutathione level. Lycopene treatment also ameliorated the IR-induced tissue damage in bilateral testes. In conclusion, the therapeutic antioxidant effect of lycopene on germ cells could serve as a promising intervention to oxidative stress-associated infertility problems, such as testicular torsion.
Role of Combined Antioxidants
Chapter · September 2014 with 8 Reads
DOI 10.1007/978-3-319-10259-7_4
Abstract: Evidence in the literature supported the use of combined antioxidants for the management of free radicals and OS prevention. The effectiveness of combined non-enzymatic antioxidants was investigated in male patients with male factor infertility prior to their third IUI treatment cycle (Dashti et al. 2013). Prior to the treatment, the males were advised to take a combination of tamoxifen 10 mg twice a day, vitamin E 400 IU daily, zinc 15 mg twice a day and selenium 200 mg daily for 3 months. The results of the study detected significant differences in overall values for the four semen parameters (sperm concentration, motility, forward progression and the percentage normal forms) in comparison to the earlier two IUI cycles in the same group. The grouping of the female patients according to their Body Mass Index (BMI) showed crucial differences in pregnancy outcome. The influence of oral antioxidant supplementation on semen quality of IVF patients undergoing IVF/ICSI was analysed in an experiment in which the male patients were supplemented with an oral antioxidant called FertilovitRMplus twice daily for 2 months (Wirleitner et al. 2012). The components of FertilovitRMplus included: Vitamin C 100 mg, Vitamin E 100 mg, Folic acid 500 μg, Zinc 25 mg, Selenium 100 μg, N-acetyl-l-Cysteine 50 mg, l-Carnitine 300 mg, Citrulline 300 mg, Glutathione red 50 mg, Lycopene 4 mg and Coenzyme Q10 15 mg. The results of this study revealed significant reduction in the percentage of immotile sperms in the patients. Additionally, the percentage of class I spermatozoa was significantly higher with drastic improvement in sperm motility as well as in total sperm count.
Role of Combined Antioxidants | Request PDF. Available from: https://www.researchgate.net/publication/301955043_Role_of_Combined_Antioxidants?ev=publicSearchHeader&_sg=Ry6PRvcYrZpToF4XB7RwWdTx_59O6ILjYuhVtM9i0mg-90Qhcte1u_bDoN2Kboh8PpbLkr_UFB7nMgs
Lycopene and male infertility
Damayanthi Durairajanayagam1,2, Ashok Agarwal1, Chloe Ong 1, Pallavi Prashast1
Excessive amounts of reactive oxygen species (ROS) cause a state of oxidative stress, which result in sperm membrane lipidperoxidation, DNA damage and apoptosis, leading to decreased sperm viability and motility. Elevated levels of ROS are a majorcause of idiopathic male factor infertility, which is an increasingly common problem today. Lycopene, the most potent singletoxygen quencher of all carotenoids, is a possible treatment option for male infertility because of its antioxidant properties. Byreacting with and neutralizing free radicals, lycopene could reduce the incidence of oxidative stress and thus, lessen the damagethat would otherwise be inflicted on spermatozoa. It is postulated that lycopene may have other beneficial effects via nonoxidativemechanisms in the testis, such as gap junction communication, modulation of gene expression, regulation of the cell cycle andimmunoenhancement. Various lycopene supplementation studies conducted on both humans and animals have shown promisingresults in alleviating male infertility—lipid peroxidation and DNA damage were decreased, while sperm count and viability,and general immunity were increased. Improvement of these parameters indicates a reduction in oxidative stress, and thus thespermatozoa is less vulnerable to oxidative damage, which increases the chances of a normal sperm fertilizing the egg. Humantrials have reported improvement in sperm parameters and pregnancy rates with supplementation of 4–8 mg of lycopene daily for3–12 months. However, further detailed and extensive research is still required to determine the dosage and the usefulness oflycopene as a treatment for male infertility.
Asian Journal of Andrology
(2014)
16
, 420–425; doi: 10.4103/1008-682X.126384; published online: 18 March 2014
https://www.scribd.com/document/299558193/24675655
Male Infertility: The Effect of Natural Antioxidants and Phytocompounds on Seminal Oxidative Stress.
Adewoyin M1, Ibrahim M2, Roszaman R3, Isa MLM4, Alewi NAM5, Rafa AAA6, Anuar MNN1.
Abstract: Defective sperm function has been identified as the most common cause of infertility. The objective of this study was to review recent findings on the effects of various antioxidants on male fertility. High amounts of poly unsaturated fatty acid are found in the mammalian spermatozoamembranes, thereby making them susceptible to lipid peroxidation. Although, free radicals and reactive oxygen species (ROS) play major roles in reproduction, they are strongly associated with oxidative stress. Furthermore, factors such as obesity, inflammation, pollutants and cigarette smoking are negatively correlated with spermatogenesis. Endogenous antioxidants system exists to mediate these damages. In a normal physiological state, the seminal plasma contains antioxidant enzyme mechanism that is capable of quenching these ROS as well as protecting the spermatozoa against any likely damage. However, high level of ROS triggered by inflammatory cells and oxidation of fatty acid in obese subjects may down play antioxidant mechanism resulting in oxidative stress. Evaluation of such oxidative stress is the first step in the treatment of male infertility through administration of suitable antioxidant. Notably, antioxidant such as vitamin E and C, carotenoids and carnitine have been found beneficial in restoring a balance between ROS generation and scavenging activities. There are emerging evidences that herbal products can also boost male reproductive functions. Nonetheless, a good lifestyle, regular exercise, avoidance of stress and observing safety rules at work are habits that can reverse male infertility.
https://www.ncbi.nlm.nih.gov/pubmed/28933362
Fertilichron female Research:
Critical Reviews in Food Science and Nutrition, 44:559–573 (2004) Copyright C Taylor and Francis Inc. ISSN: 1040-8398 DOI: 10.1080/10408690490931420
Stability and Synergistic Effect of Antioxidative Properties of Lycopene and Other Active Components
Introduction: Carotenoids have drawn considerable interest, due to their role in preventing cardiovascular disease. In a large prospective study of female nurses, a 26% and 20% lower risk of coronary artery disease was observed among the subjects in the higher quintile of β-carotene and α-carotene intake over a 12 year, follow-up period, respectively, compared with those in the lower quintile (Osganian et al., 2003). In vitro studies have indicated that carotenoids may prevent the initiating events in atherogenesis by directly inhibiting low density lipoprotein (LDL) oxidation, thereby decreasing the early formation of foam cells and plaque (Diaz et al., 1997; Maxwell and Lip, 1997; Naruszewicz et al., 1992; van de Vijver et al., 1997). The incubation of the β-carotene isomers with whole plasma resulted in substantial carotene binding to very low density lipoprotein (VLDL) and to LDL, although limited binding was observed in high density lipoprotein (HDL). Lipid peroxidation of VLDL and LDL was significantly decreased by β-carotene. In addition, the incubation of β-carotene also decreased macrophages mediated cellular degradation of oxidized lipoproteins by 18% (Lavy et al., 1993). The oxidatively modified form, but not native LDL, is Address correspondence to John Shi, Food Research Center, Agriculture and Agri-Food Canada, 93 Stone Rd. West, Guelph, Ontario NIG 5C9, Canada. E-mail: shij@agr.gc.ca preferably recognized by the receptor and could, therefore, be taken up by tissue macrophages to induce the fatty-streak lesion of atherosclerosis. More than 600 carotenoids have been found in plants and microorganisms, and many of these carotenoids have been identified in human blood and tissues. The chemical and biological function of carotenoids is determined by their characteristic structure. Lycopene is a member of the carotenoid family, and it is the naturally occurring compound that gives the characteristic red color to the tomato, watermelon, pink grapefruit, orange, and apricot. Carotenoids have important roles in photosynthesis. For example, they protect the photosynthetic system from photo-oxidative damage by quenching chlorophyll triplet states and the singlet oxygen generated, they also function as lightharvesting pigments in the antenna system of the photosynthetic organism. In addition to its function as a pigment, lycopene also is strong antioxidant, able to neutralize free radicals generated from oxygen.
Fertilichron male Research:
Effect of maca supplementation on bovine sperm quantity and quality followed over two spermatogenic cycles
(n=78, double blind, placebo controlled animal study for 10 weeks).
Clement Cet al; Theriogenology 2010
Abstract: Maca (Lepidium meyenii Walpers), is an Andean crop that grows between 3,800 and 4,500 m a.s.l. The persistent interest in this plant is based on its assumed effects on fertility of male mammals due to the prevalence of certain, partially specific, secondary compounds. The present study aimed at evaluating the effect of maca supplementation on quality and quantity of semen, mating behavior, and clinical status of peripubertal breeding bulls. The experiment followed a cross-over design lasting for 23 wk with 3 wk of adaptation and baseline measurements, and 2 x 10 wk of treatment feeding thus covering two times the complete 8-wk spermatogenic cycle. Seventy-eight 55 wk to 84 wk old breeding bulls received either no maca (control) or maca (233 mg dried hypocotyls/kg body weight/day) for 10 wk followed by 10 wk without maca (maca early) or maca only in the last 10 wk (maca late). Measurements were always made in the last 2 wk of each period. Apart from standard analyses, ejaculates were analyzed by flow cytometry. Data was evaluated by analysis of variance considering the repeated measurement structure of the data. Significant treatment by measurement period indicated direct or carry-over effects of maca. Maca supplementation had no direct effect on body weight, testes circumference, rectal temperature, mating behavior, and ejaculate volume. However, supplementing maca in the first 10 wk period increased the number of sperms in the second 10 wk period, i.e., when the animals no longer received maca. The DNA fragmentation index and the visually assessed motility of the sperms of bulls, that initially showed a borderline sperm quality, were significantly improved with early maca supplementation, while no such effect was observed in the two other groups. No effects occurred in the proportion of intact sperm plasma membranes or acrosomes or both. In conclusion, maca supplementation seems to improve sperm quantity and quality of bulls to a certain degree, while mating behavior appears unaffected.
Effect of maca supplementation on bovine sperm quantity and quality followed over two spermatogenic cycles | Request PDF. Available from: https://www.researchgate.net/publication/44582093_Effect_of_maca_supplementation_on_bovine_sperm_quantity_and_quality_followed_over_two_spermatogenic_cycles
Effect of short-term and long-term treatments with three ecotypes of Lepidium meyenii (MACA) on spermatogenesis in rats
(n=78, double blind, paralell group animal study for 42 days).
Gonzales Cet al; J Ethnopharmacol 2006
Abstract: Lepidium meyenii (Brassicaceae), known as Maca, is a Peruvian hypocotyl that grows exclusively between 4000 and 4500 m above sea level in the central Andes. Maca is traditionally employed in the Andean region for its supposed fertility-enhancing properties. The study aimed to test the hypothesis that different ecotypes of Maca (Red, Yellow and Black) after short-term (7 days) and long-term (42 days) treatment affects differentially spermatogenesis adult rats. After 7 days of treatment with Yellow and Red Maca, the length of stage VIII was increased (P < 0.05), whereas with Black Maca stages II–VI and VIII were increased (P < 0.05). Daily sperm production (DSP) was increased in the group treated with Black Maca compared with control values (P < 0.05). Red or Yellow Maca did not alter DSP and epididymal sperm motility was not affected by treatment with any ecotype of Maca. After 42 days of treatment, Black Maca was the only ecotype that enhanced DSP (P < 0.05). Moreover, Black Maca was the only that increased epididymal sperm motility (P < 0.05). In relation to the control group, Red Maca did not affect testicular and epididymal weight nor epididymal sperm motility and sperm count; however, prostate weight was reduced (P < 0.05). Black or Yellow Maca did not affect prostate weight. In conclusion, there were differences in the biological response of the three ecotypes of Maca (Yellow, Red and Black). Black Maca appeared to have more beneficial effect on sperm counts and epididymal sperm motility.
https://www.sciencedirect.com/science/article/pii/S0378874105005520
Fertilichron female Research:
Lepidium meyenii (Maca) increases litter size in normal adult female mice.
Ruiz-Luna AC1, Salazar S, Aspajo NJ, Rubio J, Gasco M, Gonzales GF.
Abstract:
Background: Lepidium meyenii, known as Maca, grows exclusively in the Peruvian Andes over 4000 m altitude. It has been used traditionally to increase fertility. Previous scientific studies have demonstrated that Maca increases spermatogenesis and epididymal sperm count. The present study was aimed to investigate the effects of Maca on several fertility parameters of female mice at reproductive age.
Methods: Adult female Balb/C mice were divided at random into three main groups: i) Reproductive indexes group, ii) Implantation sites group and iii) Assessment of uterine weight in ovariectomized mice. Animals received an aqueous extract of lyophilized Yellow Maca (1 g/Kg BW) or vehicle orally as treatment. In the fertility indexes study, animals received the treatment before, during and after gestation. The fertility index, gestation index, post-natal viability index, weaning viability index and sex ratio were calculated. Sexual maturation was evaluated in the female pups by the vaginal opening (VO) day. In the implantation study, females were checked for implantation sites at gestation day 7 and the embryos were counted. In ovariectomized mice, the uterine weight was recorded at the end of treatment.
Results: Implantation sites were similar in mice treated with Maca and in controls. All reproductive indexes were similar in both groups of treatment. The number of pups per dam at birth and at postnatal day 4 was significantly higher in the group treated with Maca. VO day occurred earlier as litter size was smaller. Maca did not affect VO day. In ovariectomized mice, the treatment with Maca increased significantly the uterine weights in comparison to their respective control group.
Conclusion: Administration of aqueous extract of Yellow Maca to adult female mice increases the litter size. Moreover, this treatment increases the uterine weight in ovariectomized animals. Our study confirms for the first time some of the traditional uses of Maca to enhance female fertility.
https://www.ncbi.nlm.nih.gov/pubmed/15869705
Hormone-Balancing Effect of Pre-Gelatinized Organic Maca (Lepidium peruvianum Chacon): (III) Clinical responses of early-postmenopausal women to Maca in double blind, randomized, Placebo-controlled, crossover configuration, outpatient study.
Meissner HO1, Mscisz A, Reich-Bilinska H, Mrozikiewicz P, Bobkiewicz-Kozlowska T, Kedzia B, Lowicka A, Barchia I.
Abstract: This is the second, conclusive part of the clinical study on clinical responses of early-postmenopausal women to standardized doses of pre-Gelatinized Organic Maca (Maca-GO). Total of 34 Caucasian women volunteers participated in a double-blind, randomized, four months outpatient crossover configuration Trial. After fulfilling the criteria of being early-postmenopausal: blood Estrogen (E2<40 pg/ml) and Follicle Stimulating Hormone (FSH>30 IU/ml) at admission, they were randomly allocated to Placebo (P) and Maca-GO (M) treatments (2 groups of 11 participants each). Two 500 mg vegetable hard gel capsules with Maca-GO or Placebo powder were self-administered twice daily with meals (total 2 g/day). At admission and follow-up monthly intervals, body mass index (BMI), blood pressure, levels of gonadal, pituitary, thyroid and adrenal hormones, lipids and key minerals were measured. Bone markers were determined after four months M and P use in 12 participants. Menopausal symptoms were assessed according to Greene's Score (GMS) and Kupperman's Index (KMI). Data were analyzed using multivariate technique on blocs of monthly. Results and canonical variate technique was applied to GMS and KMI matrices. Two months application of Maca-GO stimulated (P<0.05) production of E2, suppressed (P<0.05) blood FSH, Thyroid (T3) and Adrenocorticotropic hormones, Cortisol, and BMI, increased (P<0.05) low density lipoproteins, blood Iron and alleviated (P<0.001) menopausal symptoms. Maca-GO noticeably increased bone density markers. In conclusion, Maca-GO applied to early-postmenopausal women (i) acted as a toner of hormonal processes along the Hypothalamus-Pituitary-Ovarian axis, (ii) balanced hormone levels and (iii) relieved symptoms of menopausal discomfort, (hot flushes and night sweating in particular), thus, (iv) exhibited a distinctive function peculiar to adaptogens, providing an alternative non-hormonal plant option to reduce dependence on hormone therapy programs (HRT).
Fertilichron male Research:
A post-publication analysis of the idealized upper reference value of 2.5 mIU/L for TSH: Time to support the thyroid axis with magnesium and iron especially in the setting of reproduction medicine.
Abstract: Laboratory medicine approaches the evaluation of thyroid function mostly through the single determination of the blood level of thyroid stimulating hormone (TSH). Some authors have suggested an upper reference value for TSH of 2.5 mIU/L. This suggestion has not been confirmed by recent clinical studies. These studies have delivered a clinically valid reference range going from 0.3 to 3.5 mIU/L. These values are valid for both for the general population as well as in the setting of fertility and pregnancy. Current biochemical evidence about the elements required to maintain thyroid function shows that these not only include dietary iodine but also magnesium, iron, selenium and coenzyme Q10. Iron is important for the synthesis of thyroid peroxidase; magnesium-ATP contributes to the active process of iodine uptake; iodine has to be sufficiently present in the diet; selenium acts through selenoproteins to protect the thyroid cell during hormone synthesis and in deiodination of thyroxine; coenzyme Q10 influences thyroid vascularity. As a consequence, good clinical practice requires additional biochemical information on the blood levels of magnesium, selenium, coenzyme Q10 as well as iron status. Since these elements are also important for the maintenance of reproductive function, we postulate that they constitute the connecting link between both endocrine systems.
https://www.ncbi.nlm.nih.gov/pubmed/28409122
Fertilichron female Research:
A post-publication analysis of the idealized upper reference value of 2.5 mIU/L for TSH: Time to support the thyroid axis with magnesium and iron especially in the setting of reproduction medicine.
Abstract: Laboratory medicine approaches the evaluation of thyroid function mostly through the single determination of the blood level of thyroid stimulating hormone (TSH). Some authors have suggested an upper reference value for TSH of 2.5 mIU/L. This suggestion has not been confirmed by recent clinical studies. These studies have delivered a clinically valid reference range going from 0.3 to 3.5 mIU/L. These values are valid for both for the general population as well as in the setting of fertility and pregnancy. Current biochemical evidence about the elements required to maintain thyroid function shows that these not only include dietary iodine but also magnesium, iron, selenium and coenzyme Q10. Iron is important for the synthesis of thyroid peroxidase; magnesium-ATP contributes to the active process of iodine uptake; iodine has to be sufficiently present in the diet; selenium acts through selenoproteins to protect the thyroid cell during hormone synthesis and in deiodination of thyroxine; coenzyme Q10 influences thyroid vascularity. As a consequence, good clinical practice requires additional biochemical information on the blood levels of magnesium, selenium, coenzyme Q10 as well as iron status. Since these elements are also important for the maintenance of reproductive function, we postulate that they constitute the connecting link between both endocrine systems.
https://www.ncbi.nlm.nih.gov/pubmed/28409122
Dietary minerals, reproductive hormone levels and sporadic anovulation: associations in healthy women with regular menstrual cycles.
Kim K1, Wactawski-Wende J2, Michels KA1, Schliep KC3, Plowden TC1, Chaljub EN1, Mumford SL1.
Abstract: Although minerals are linked to several reproductive outcomes, it is unknown whether dietary minerals are associated with ovulatory function. We hypothesised that low intakes of minerals would be associated with an increased risk of anovulation. We investigated associations between dietary mineral intake and both reproductive hormones and anovulation in healthy women in the BioCycle Study, which prospectively followed up 259 regularly menstruating women aged 18-44 years who were not taking mineral supplements for two menstrual cycles. Intakes of ten selected minerals were assessed through 24-h dietary recalls at up to four times per cycle in each participant. Oestradiol, progesterone, luteinising hormone (LH), follicle-stimulating hormone (FSH), sex-hormone-binding globulin and testosterone were measured in serum up to eight times per cycle. We used weighted linear mixed models to evaluate associations between minerals and hormones and generalised linear models for risk of anovulation. Compared with Na intake ≥1500 mg, Na intake <1500 mg was associated with higher levels of FSH (21·3 %; 95 % CI 7·5, 36·9) and LH (36·8 %; 95 % CI 16·5, 60·5) and lower levels of progesterone (-36·9 %; 95 % CI -56·5, -8·5). Na intake <1500 mg (risk ratio (RR) 2·70; 95 % CI 1·00, 7·31) and Mn intake <1·8 mg (RR 2·00; 95 % CI 1·02, 3·94) were associated with an increased risk of anovulation, compared with higher intakes, respectively. Other measured dietary minerals were not associated with ovulatory function. As essential minerals are mostly obtained via diet, our results comparing insufficient levels with sufficient levels highlight the need for future research on dietary nutrients and their associations with ovulatory cycles.
Keywords: Ca; Cu; FSH follicle-stimulating hormone; Fe; K; LH luteinising hormone; Mg; Mn; Na; P; Se; Zn; calcium; copper; iron; magnesium; manganese; phosphorus; potassium; selenium; sodium; zinc; Anovulation; Dietary minerals; Premenopausal women; Reproductive hormones
https://www.ncbi.nlm.nih.gov/pubmed/29673411
Assessment of dietary intake and mineral status in pregnant women.
Kocyłowski R1,2, Lewicka I3, Grzesiak M4, Gaj Z1,5, Sobańska A3, Poznaniak J3, von Kaisenberg C6, Suliburska J7.
Abstract:
Purpose: To evaluate the dietary intake of pregnant women and their nutritional status of Ca, Mg, Fe, Zn, and Cu, as the nutritional status of pregnant women is an important factor for the proper progression of a pregnancy and the development and health of the fetus.
Methods: The study was conducted on 108 pregnant women ages 18-42, at 6-32 weeks of gestation. We used a questionnaire and a 24-h recall nutrition interview. Hair samples were taken for testing and the level of each mineral was assessed using atomic absorption spectrometry. The results were analysed using the Dietetyk and Statistica 10 software.
Results: Low levels of Fe, Zn, Ca, Mg, vitamin D, and folic acid intake were seen in the pregnant women, with the use of dietary supplements significantly increasing their intake of Fe, Zn, and folic acid. The concentration of zinc and magnesium in the women's hair was shown to be affected by their age and, in the case of magnesium, by the week of pregnancy.
Conclusions: It was observed that the diet of pregnant women is characterized by low levels of Fe, Zn, Ca, Mg, vitamin D, and folic acid. Dietary supplementation with vitamins and minerals significantly increases the daily Fe and folic acid intake in pregnant women. The concentration of Zn and Mg in hair depends on the age of pregnant women and Mg level in the hair of women decreases during pregnancy.
Fertilichron male Research:
Multivitamin and micronutrient treatment improves semen parameters of azoospermic patients with maturation arrest
(n=35, double blind, placebo controlled trail for 3 month).
Singh AKet al., Indian J Physiol Pharmacol 2010
Abstract : The study was undertaken to evaluate the efficacy of multivitamin and micronutrient supplementation in azoospermic patients with maturation arrest. A total of 35 azoospermic patients showing maturation arrest on testicular biopsy were recruited in this study. The patients were divided into two groups. Untreated group (n=11) without any treatment and treated group (n=24) who received multivitamins, micronutrients and co-enzyme Q10. The sperm concentration, motility and morphology were evaluated at monthly interval. The results showed reduction in liquefaction time and relative viscosity of the semen in the treated group . Further, in treated group there was appearance of spermatozoa (4.0 million/ml) exhibiting progressive motility (7%) and normal morphology (6%), even in the first follow up visit. The sperm count, motility and normal morphology increased significantly on subsequent visits. Within 3 months (3 visits) 2 pregnancies were reported. These observations indicate that multivitamin and micronutrient supplementation improve the qualitative and quantitative parameters of seminogram in patients with azoospermia of maturation arrest.
Lipovac M, Bodner F, Imhof M, Chedraui P.
Reprod Biol Endocrinol.2016 Dec 9;14(1):84.
Comparison of the effect of a combination of eight micronutrients versus a standard mono preparation on sperm parameters.
Abstract:
Background: There are reports showing that l-carnitine alone or in combination with other micronutrients improve sperm parameters. However, comparative studies are still lacking. This study was carried out to compare the short term effects of a combination of eight micronutrients including l-carnitine vs. a mono-substance (l-carnitine alone) on sperm parameters.
Methods: This was a prospective, open-labelled, nonrandomized study that included male subjects (20 to 60 years) with at least 1 year of subfertility and at least one pathological semen analysis who received 3 months treatment with a mono-substance (500 mg l-carnitine/twice a day, n = 156) or a combined compound (440 mg l-carnitine + 250 mg l-arginine + 40 mg zinc + 120 mg vitamin E + 80 mg glutathione + 60 μg selenium + 15 mg coenzyme Q10 + 800 μg folic acid/once a day, n = 143) for the same time period. Sperm parameters were analyzed before and after treatment and groups comparisons performed.
Results: Baseline characteristics were similar among studied groups (age and body mass indices). Semen parameters (volume, density, overall progressive motility [including slow and fast motility]) and percentage of sperm with normal morphology improved after 3 months in both groups as compared to baseline. However, relative change (expressed as % increase of absolute values) for sperm density and overall progressive motility (including fast motility) was found to be higher for the combined micronutrient treatment group as compared to the mono-treatment using l-carnitine alone.
Conclusions: Both analyzed groups displayed a positive short term effect on all sperm parameters; however effect on density and motility was significantly better for the combined formulation. There is need for more research in this matter that includes long term outcome data.
Azizollahi G, Azizollahi S, Babaei H, Kianinejad M, Baneshi MR, Nematollahi-mahani SN.
J Assist Reprod Genet.2013 Apr;30(4):593-9. doi: 10.1007/s10815-013-9961-9. Epub 2013 Feb 24.
Effects of supplement therapy on sperm parameters, protamine content and acrosomal integrity of varicocelectomized subjects.
Abstract:
Purpose: Surgical repair of varicocele has long been a procedure to correct spermatogenesis. However, the outcome has been reported to be inadequate. We combined varicocelectomy with supplement therapy to evaluate the concurrent effect of these procedures.
Methods: A prospective randomized controlled study was undertaken to investigate the effects of zinc sulfate, folic acid and zinc sulfate/folic acid on sperm quality, protamine content and acrosomal integrity following surgical repair of varicocele. Male subjects with palpable varicocele were included in the study and randomized into four groups. Subjects received Zinc sulfate, Folic acid, Zinc sulfate/Folic acid or placebo for 6 months. A semen sample was obtained before surgery and 3 and 6 months after surgical repair. Semen samples were evaluated for sperm parameters as well as chromatin content and acrosomal integrity.
Results: Most of the evaluated parameters showed a mild improvement after varicocelectomy in the placebo group. Interestingly, co-administration of Zinc sulfate and folic acid improved most factors significantly. Folic acid administration but not zinc sulfate could increase sperm number. Hence, Zinc sulfate was better than folic acid when change in morphology was assessed, and none of them was significantly effective in sperm motility. In Zinc sulfate and Folic acid groups, protamine content and halo formation rate significantly improved.
Conclusions: We may conclude that co-administration of zinc and folic acid significantly improved sperm parameters and increased varicocelectomy outcomes. So, medical treatment with compatible drugs after surgery might be advantageous for obtaining acceptable results.
Young SS, Eskenazi B, Marchetti FM, Block G, Wyrobek AJ.
Hum Reprod.2008 May;23(5):1014-22. doi: 10.1093/humrep/den036. Epub 2008 Mar 19.
The association of folate, zinc and antioxidant intake with sperm aneuploidy in healthy non-smoking men.
Abstract:
Background: Little is known about the effect of paternal nutrition on aneuploidy in sperm. We investigated the association of normal dietary and supplement intake of folate, zinc and antioxidants (vitamin C, vitamin E and beta-carotene) with the frequency of aneuploidy in human sperm.
Methods: Sperm samples from 89 healthy, non-smoking men from a non-clinical setting were analyzed for aneuploidy using fluorescent in situ hybridization with probes for chromosomes X, Y and 21. Daily total intake (diet and supplements) for zinc, folate, vitamin C, vitamin E and beta-carotene was derived from a food frequency questionnaire. Potential confounders were obtained from a self-administered questionnaire.
Results: After adjusting for covariates, men with high folate intake (>75th percentile) had lower frequencies of sperm with disomies X, 21, sex nullisomy, and a lower aggregate measure of sperm aneuploidy (P <or= 0.04) compared with men with lower intake. In adjusted continuous analyses, total folate intake was inversely associated with aggregate sperm aneuploidy (-3.6% change/100 microg folate; 95% CI: -6.3, -0. 8) and results were similar for disomies X, 21 and sex nullisomy. No consistent associations were found between antioxidant or zinc intakes and sperm aneuploidy.
Conclusions: Men with high folate intake had lower overall frequencies of several types of aneuploid sperm.
J Nutr Sci Vitaminol (Tokyo).2012;58(4):230-9.
The interactive effect of dietary water-soluble vitamin levels on the depression of gonadal development in growing male rats kept under disturbed daily rhythm.
Abstract: The purpose of this study was to clarify the effects of nutrients on the gonadal development of male rats kept under constant darkness as a model of disturbed daily rhythm. In the present study we examined the effects of nine water-soluble vitamins. We selected 7 water-soluble vitamins (choline, nicotinic acid (NA), pantothenic acid (PA), vitamin B6 (VB6), vitamin B1 (VB1), vitamin B2 (VB2) and folic acid (FA)) as experimental factors for the first experiment (Ex. 1) and biotin and vitamin B12 (VB12) as experimental factors for the second experiment (Ex. 2). The dietary content of these vitamins was normal or six times the normal content. Lighting condition (L.C.) was also added as a factor. Four-week-old male rats (Fischer 344 strain) were kept under constant darkness or normal lighting (12-h light/dark cycle) for 4 wk. The depression of gonadal development in the constant darkness groups (D-groups) was shown. The L.C., PA, VB6 and VB1 influenced testes development, and these three vitamins had interactions with L.C. Among the normal lighting groups (N-groups), the highest value for testes weight was observed under the normal-PA, high-VB6 and high-B1 diet; on the other hand, among the D-groups, it was observed under the high-PA, normal-VB6 and normal-VB1 diet. The results showed that the depression of gonadal development in rats kept under disturbed daily rhythm was improved by getting a high amount of PA and normal amount of VB6 and VB1.
Trace Element Deficiencies and Fertility in Ruminants: A Review
Article · Literature Review in Journal of Dairy Science 62(8):1195-206 · September 1979 with 204 Reads
DOI: 10.3168/jds.S0022-0302(79)83400-1 · Source: PubMed
Abstract: Various minerals (copper, cobalt, selenium, manganese, iodine, zinc, and iron) can influence reproductive performance of ruminants. Reproductive failure may be induced by deficiencies of single or combined trace elements and by imbalances. This review is focused on maladjustments of trace elements leading to impaired breeding performance. Opinion is diverse as to the existence of various reproductive disturbances from either a severe copper depletion or a marginal dietary copper deficiency. Field experience suggests that administration of cobalt to ruminants on cobalt-deficient diets improves their impaired breeding performance. Selenium infertility in ewes is more prevalent in some areas and in some seasons, but the actual cause of this malady and the continuing role of additional factors are unknown. Manganese is necessary for normal fertility in ruminants, and feeding low-manganese rations depresses conception rates. Lack of iodine impairs thyroid activity and also ovarian function. Reproductive failure in the female and in spermatogenesis are manifestations of zinc deficiency. Despite forages rich in iron, low availability in certain instances could affect adversely ruminant reproduction. Knowledge of biochemical dysfunctions from trace element deficiencies is essential to determine the role which trace elements play in fertility of ruminant animals.
Trace Element Deficiencies and Fertility in Ruminants: A Review. Available from: https://www.researchgate.net/publication/22753545_Trace_Element_Deficiencies_and_Fertility_in_Ruminants_A_Review?_sg=ePG6R0QZjJ37LsndCHejvoTla3L0VHCkKnJwx_I6pOuSAsRj0d7MTwZ4B5HPSq3R7HDSDeqVY0IsDFs
One-carbon cycle support rescues sperm damage in experimentally induced varicocoele in rats.
Mohammadi P1,2, Hassani-Bafrani H2,3, Tavalaee M1, Dattilo M4, Nasr-Esfahani MH1,5.
Abstract:
Objectives: To investigate whether micronutrients in support of the one-carbon cycle and glutathione synthesis are effective in improving sperm damage after surgical varicocoele induction in rats and whether any effect is achieved without a rebound reductive stress as seen with oral antioxidants.
Materials and Methods: Surgical varicocoele was induced in adult male Wistar rats and resulted in significant damage to the testis and sperm cells measured at 2 and 4 months after surgery. At 2 months after surgery, rats received a 2-month oral supplementation in support of the one-carbon cycle containing B vitamins (B2, B3, B6, folic acid and B12), N-acetyl-cysteine, zinc, small amounts of vitamin E, and a natural source of betalains and quercetine (Condensyl® ; Parthenogen SAGL, Lugano, Switzerland and Nurilia SARL, Lyon, France).
Results: One-carbon cycle supplementation, compared to untreated controls, significantly improved the morphometric characteristics of testis (P < 0.05), sperm concentration, motility and abnormal morphology (P < 0.001), sperm chromatin condensation (aniline blue staining, P < 0.05), sperm DNA damage (acridine orange staining, P < 0.05) and sperm lipid peroxidation (BODIPY C11, P < 0.001). The improvement in both nuclear condensation and DNA damage and the lack of excessive inhibition of lipid peroxidation confirmed that no reductive stress had occurred.
Conclusions: Micronutrients in support of the one-carbon cycle are effective in the treatment of surgically induced varicocoele in rats, probably by activating natural antioxidant defenses and epigenetics. These results support the idea that essential micronutrients including B vitamins may also have a positive influence in clinical varicocoele, which should be tested in prospective clinical trials.
https://www.ncbi.nlm.nih.gov/pubmed/29752770
Dietary patterns, foods and nutrients in male fertility parameters and fecundability: a systematic review of observational studies.
Salas-Huetos A1,2, Bulló M1,2, Salas-Salvadó J1,2.
Abstract:
Background: Infertility is a global public health issue, affecting 15% of all couples of reproductive age. Male factors, including decreased semen quality, are responsible for ~25% of these cases. The dietary pattern, the components of the diet and nutrients have been studied as possible determinants of sperm function and/or fertility.
Objective and Rationale: Previous systematic reviews have been made of the few heterogeneous low-quality randomized clinical trials (RCTs) conducted in small samples of participants and investigating the effect of specific nutrients and nutritional supplements on male infertility. However, as yet there has been no systematic review of observational studies.
Search Methods: A comprehensive systematic review was made of the published literature, from the earliest available online indexing year to November 2016, in accordance with the guidelines of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses. We have included cross-sectional, case-control and prospective and retrospective studies in which fertile/infertile men were well defined (men with sperm disorders, sperm DNA damage, varicocele or idiopathic infertility). The primary outcomes were semen quality or fecundability. With the data extracted, we evaluated and scored the quality of the studies selected. We excluded RCTs, animal studies, review articles and low-quality studies.
Outcomes: A total of 1944 articles were identified, of which 35 were selected for qualitative analysis. Generally, the results indicated that healthy diets rich in some nutrients such as omega-3 fatty acids, some antioxidants (vitamin E, vitamin C, β-carotene, selenium, zinc, cryptoxanthin and lycopene), other vitamins (vitamin D and folate) and low in saturated fatty acids and trans-fatty acids were inversely associated with low semen quality parameters. Fish, shellfish and seafood, poultry, cereals, vegetables and fruits, low-fat dairy and skimmed milk were positively associated with several sperm quality parameters. However, diets rich in processed meat, soy foods, potatoes, full-fat dairy and total dairy products, cheese, coffee, alcohol, sugar-sweetened beverages and sweets have been detrimentally associated with the quality of semen in some studies. As far as fecundability is concerned, a high intake of alcohol, caffeine and red meat and processed meat by males has a negative influence on the chance of pregnancy or fertilization rates in their partners.
Wider Implications: Male adherence to a healthy diet could improve semen quality and fecundability rates. Since observational studies may prove associations but not causation, the associations summarized in the present review need to be confirmed with large prospective cohort studies and especially with well-designed RCTs.
https://www.ncbi.nlm.nih.gov/pubmed/28333357
Fertilichron female Research:
Role of reducing fertility factors in reproductive aged women and their assosiation with micronutrients
Article · October 2016 with 2 Reads
DOI: 10.18370/2309-4117.2016.31.40-48
Abstract: Fertility is ability of sexually mature organism to reproduce offspring. Infertility is an inability of organism to conceive a mature. The frequency of male and female factors is above 40% in the structure of marriage infertility, 15% of infertility causes is caused by both partners, 5–10% of cases are not established. The most common causes of female infertility are an ovulation disorders (25–30%) and tubal occlusion (20–25%). Stress is one of the probable cases of the fertility decline and insufficient effectiveness of the reproductive programs, especially for unknown origin. Hypothalamic-pituitary-adrenal system, which leads to stress reaction, can significantly inhibit the function of the female reproductive system at different levels. Oxidative stress in the ovaries is another important mechanism to reduce fertility. No one doubts that a deficiency of vitamins and elements can reduce fertility and cause infertility. Since impaired fertility involved a number of known active substances, during the infertility treatment should take into account this factor and to include those macro- and microelements and vitamins, the probability of which deficiency is the highest. They include homocysteine, folate, vitamin E, vitamin C, group B vitamins, L-arginine, magnesium, zinc, selenium, and others. According to many publications appointment of the trace elements and vitamins, which are lacking in the body, provides the adaptation of the nervous system, hormonal homeostasis and the optimal condition of the reproductive system organs prior to pregnancy. Physician should be carefully weighed hormone therapy at the fertile period of woman, based on the benefits and risks for the woman and for the unborn child. This hormonal therapy, as a necessary component in patients with endocrine infertility or women in program of assisted reproductive technologies may not have the expected success due to the formation of micronutrient deficiency.
Role of reducing fertility factors in reproductive aged women and their assosiation with micronutrients. Available from: https://www.researchgate.net/publication/312248124_Role_of_reducing_fertility_factors_in_reproductive_aged_women_and_their_assosiation_with_micronutrients
Trace Element Deficiencies and Fertility in Ruminants: A Review
Article · Literature Review in Journal of Dairy Science 62(8):1195-206 · September 1979 with 204 Reads
DOI: 10.3168/jds.S0022-0302(79)83400-1 · Source: PubMed
Abstract: Various minerals (copper, cobalt, selenium, manganese, iodine, zinc, and iron) can influence reproductive performance of ruminants. Reproductive failure may be induced by deficiencies of single or combined trace elements and by imbalances. This review is focused on maladjustments of trace elements leading to impaired breeding performance. Opinion is diverse as to the existence of various reproductive disturbances from either a severe copper depletion or a marginal dietary copper deficiency. Field experience suggests that administration of cobalt to ruminants on cobalt-deficient diets improves their impaired breeding performance. Selenium infertility in ewes is more prevalent in some areas and in some seasons, but the actual cause of this malady and the continuing role of additional factors are unknown. Manganese is necessary for normal fertility in ruminants, and feeding low-manganese rations depresses conception rates. Lack of iodine impairs thyroid activity and also ovarian function. Reproductive failure in the female and in spermatogenesis are manifestations of zinc deficiency. Despite forages rich in iron, low availability in certain instances could affect adversely ruminant reproduction. Knowledge of biochemical dysfunctions from trace element deficiencies is essential to determine the role which trace elements play in fertility of ruminant animals.
Trace Element Deficiencies and Fertility in Ruminants: A Review. Available from: https://www.researchgate.net/publication/22753545_Trace_Element_Deficiencies_and_Fertility_in_Ruminants_A_Review?_sg=ePG6R0QZjJ37LsndCHejvoTla3L0VHCkKnJwx_I6pOuSAsRj0d7MTwZ4B5HPSq3R7HDSDeqVY0IsDFs
The effect of micronutrient supplements on female fertility.
Abstract:
Purpose of Review: Benefit of micronutrient supplementation on female fertility.
Recent Findings: Reports of randomized trials are rare. Most studies are focused on multivitamin supplementations. For some micronutrients, a positive impact on fertility could be shown. This article reviews the available clinical studies as well as the pathophysiological background of possible effects and summarizes the potential benefits of selected micronutrients on female fertility.
Summary: Apart from lowering the malformation risk by periconceptional supplementation of folic acid, substitution with different micronutrients, particularly folic acid, vitamin B6, vitamin C, vitamin D, vitamin E, iodine, selenium, iron, and DHA might have a positive impact on infertility treatment. The multivitamin formulation should take the pathophysiology, clinical studies, and upper limits into account.
Fertilichron male Research:
Effect of omega-3 polyunsaturated fatty acid supplementation on semen profile and enzymatic anti-oxidant capacity of seminal plasma in infertile men with idiopathic oligoasthenoteratospermia: a double-blind, placebo-controlled, randomised study
(n=238, double blind, placebo controlled trail per 32 weeks).
Safarinejad MR; Andrologia 2011
Abstract: Effective medical treatments of infertile men with idiopathic oligoasthenoteratospermia (OAT) have yet to be determined. This study considered two major aims: (i) to measure the changes in semen parameters, omega-3 fatty acids (FA) compositions and anti-oxidant activity; (ii) to determine if the administration of omega-3 FA affect semen quality in infertile men with OAT. Two hundred thirty-eight infertile men with idiopathic OAT were randomised to eicosapentaenoic (EPA) and docosahexaenoic acids (DHA), 1.84 g per day (EPAX 5500TG; Lysaker, Norway), or placebo for 32 weeks. The semen parameters were assessed according to WHO criteria, and the EPA and DHA concentrations were determined in red blood cells (RBCs), seminal plasma and sperm cells at baseline and 32-week treatment period. Of randomised subjects, 211 (88.7%) completed the full 32-week randomisation period. The anti-oxidant status of seminal plasma was also evaluated by measuring the superoxide dismutase (SOD) and catalase-like activity. In the total group of participants, all EPA and DHA levels in RBC, and seminal plasma, were statistically significantly correlated with those in spermatozoa (both P = 0.001). A significant improvement of sperm cell total count (from 38.7 ± 8.7 ' 10⁶to 61.7 ± 11.2 ' 10⁶, P = 0.001) and sperm cell concentration (from 15.6 ± 4.1 ' 10⁶per ml to 28.7 ± 4.4 ' 10⁶per ml, P = 0.001) was observed in the omega-3 group. A significant positive correlation was found between the EPA and DHA in seminal plasma and the semen parameters. Seminal plasma EPA and DHA concentrations were positively correlated with seminal plasma SOD-like and catalase-like activity (both P = 0.001). In seminal plasma, both SOD-like and catalase-like activity were positively correlated with sperm count, sperm motility, and sperm morphology. Oligoasthenoteratospermic men with low levels of EPA and DHA may benefit from omega-3 FA supplementation. Further studies are warranted to shed more light on this important issue.
Relationship of omega-3 and omega-6 fatty acids with semen characteristics, and anti-oxidant status of seminal plasma: a comparison between fertile and infertile men
(n=82 infertile and 87 fertile, epidemiological study).
Safarinejad MR et al; Clin Nutr 2010 Feb
Abstract:
Background and Aims: Fatty acid (FA) composition of the spermatozoa may be an important determinant of fertility. The aim was to evaluate polyunsaturated fatty acid (PUFA) composition of the blood plasma and spermatozoa in infertile men with idiopathic oligoasthenoteratozoospermia (OAT).
Methods: Eighty-two infertile men with idiopathic OAT and seventy-eight fertile men defined according to semen concentration and proven fertility were enrolled in the study. The semen parameters were assessed according to World Health Organization criteria; three omega-3 fatty acids--alpha-linolenic acid (ALA), eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA), and two omega-6 fatty acids--linoleic acid (LA) and arachidonic acid (AA) concentrations were measured in blood plasma and spermatozoa; and the seminal plasma enzymatic antioxidant levels of catalase, and superoxide dismutase (SOD) were also assessed.
Results: Proven fertile men had higher blood and spermatozoa levels of omega-3 FAs compared with the infertile patients. The ratio of serum omega-6/omega-3 fatty acids was significantly higher in infertile (14.8+/-4.3) patients compared to fertile controls (6.3+/-2.2) (P=0.001). Additionally, levels of AA were higher and the omega-3 index (EPA+DHA) was lower in infertile subjects than in fertile controls (all P values<0.05). Infertile men had higher mean AA:DHA ratio and AA:EPA (6.4+/-2.9 and 12.0+/-4.9, respectively) than fertile men (3.3+/-1.8 and 6.7+/-2.6, respectively) (both P=0.001). A strong negative correlation was found between the AA:DHA and AA:EPA ratios and total sperm count (r=-0.62, P=0.001 and r=-0.64, P=0.001, respectively), sperm motility (r=-0.63, P=0.001 and r=-0.61, P=0.001, respectively), and sperm morphology (r=-0.61, P=0.001, and r=-0.59, P=0.002, respectively).
Conclusions: Infertile men had lower concentrations of omega-3 FAs in spermatozoa than fertile men. These results suggest that research should be performed to assess the potential benefits of omega-3 FA supplementation as a therapeutic approach in infertile men with idiopathic OAT.
Fertilichron female Research:
A combined supplementation of omega-3 fatty acids and micronutrients (folic acid, vitamin B12) reduces oxidative stress markers in a rat model of pregnancy induced hypertension.
Kemse NG1, Kale AA1, Joshi SR1.
Abstract:
Objectives: Our earlier studies have highlighted that an altered one carbon metabolism (vitamin B12, folic acid, and docosahexaenoic acid) is associated with preeclampsia. Preeclampsia is also known to be associated with oxidative stress and inflammation. The current study examines whether maternal folic acid, vitamin B12 and omega-3 fatty acid supplementation given either individually or in combination can ameliorate the oxidative stress markers in a rat model of pregnancy induced hypertension (PIH).
Materials and Methods: Pregnant Wistar rats were assigned to control and five treatment groups: PIH; PIH + vitamin B12; PIH + folic acid; PIH + Omega-3 fatty acids and PIH + combined micronutrient supplementation (vitamin B12 + folic acid + omega-3 fatty acids). L-Nitroarginine methylester (L-NAME; 50 mg/kg body weight/day) was used to induce hypertension during pregnancy. Blood Pressure (BP) was recorded during pregnancy and dams were dissected at d20 of gestation.
Results: Animals from the PIH group demonstrated higher (p<0.01 for both) systolic and diastolic BP; lower (p<0.01) pup weight; higher dam plasma homocysteine (p<0.05) and dam and offspring malondialdehyde (MDA) (p<0.01), lower (p<0.05) placental and offspring liver DHA and higher (p<0.01) tumor necrosis factor-alpha (TNF-ά) levels as compared to control. Individual micronutrient supplementation did not offer much benefit. In contrast, combined supplementation lowered systolic BP, homocysteine, MDA and placental TNF-ά levels in dams and liver MDA and protein carbonyl in the offspring as compared to PIH group.
Conclusion: Key constituents of one carbon cycle (folic acid, vitamin B12 and DHA) may play a role in reducing oxidative stress and inflammation in preeclampsia.
https://www.ncbi.nlm.nih.gov/pubmed/25405347
The periconceptional period, reproduction and long-term health of offspring: the importance of one-carbon metabolism.
Steegers-Theunissen RP1, Twigt J, Pestinger V, Sinclair KD.
Abstract:
Background: Most reproductive failures originate during the periconceptional period and are influenced by the age and the lifestyle of parents-to-be. We advance the hypothesis that these failures can arise as a partial consequence of derangements to one-carbon (1-C) metabolism (i.e. metabolic pathways that utilize substrates/cofactors such as methionine, vitamin B12, folate). 1-C metabolic pathways drive the synthesis of proteins, biogenic amines and lipids required for early growth, together with the synthesis and methylation of DNA and histones essential for the regulation of gene expression. We review how deficiencies in periconceptional 1-C metabolism affect fertility and development together with underlying mechanisms derived from animal studies.
Methods: A literature search was performed using PubMed and bibliographies of all relevant original research articles and reviews.
Results: We define 'periconception' as a 5-6-month period in women embracing oocyte growth, fertilization, conceptus formation and development to Week 10 of gestation (coinciding with the closure of the secondary palate in the embryo). During this period significant epigenetic modifications to chromatin occur that correspond with normal development. Subtle variations in 1-C metabolism genes and deficiencies in 1-C substrates/cofactors together with poor lifestyle, such as smoking and alcohol consumption, disturb 1-C metabolism and contribute to subfertility and early miscarriage and compromise offspring health. Procedures used in assisted reproduction can also disturb these metabolic pathways and contribute to poor pregnancy outcomes.
Conclusions: Evidence presented indicates that parental nutrition and other lifestyle factors during the periconceptional period can affect reproductive performance via 1-C metabolic pathways. This knowledge provides opportunities for treatment and prevention of reproductive failures and future non-communicable diseases.
https://www.ncbi.nlm.nih.gov/pubmed/23959022
The effect of micronutrient supplements on female fertility.
Abstract:
Purpose of Review: Benefit of micronutrient supplementation on female fertility.
Recent Findings: Reports of randomized trials are rare. Most studies are focused on multivitamin supplementations. For some micronutrients, a positive impact on fertility could be shown. This article reviews the available clinical studies as well as the pathophysiological background of possible effects and summarizes the potential benefits of selected micronutrients on female fertility.
Summary: Apart from lowering the malformation risk by periconceptional supplementation of folic acid, substitution with different micronutrients, particularly folic acid, vitamin B6, vitamin C, vitamin D, vitamin E, iodine, selenium, iron, and DHA might have a positive impact on infertility treatment. The multivitamin formulation should take the pathophysiology, clinical studies, and upper limits into account.
https://www.ncbi.nlm.nih.gov/pubmed/23571830
Antioxidants for female subfertility.
Showell MG1, Mackenzie-Proctor R, Jordan V, Hart RJ.
Abstract:
Background: A couple may be considered to have fertility problems if they have been trying to conceive for over a year with no success. This may affect up to a quarter of all couples planning a child. It is estimated that for 40% to 50% of couples, subfertility may result from factors affecting women. Antioxidants are thought to reduce the oxidative stress brought on by these conditions. Currently, limited evidence suggests that antioxidants improve fertility, and trials have explored this area with varied results. This review assesses the evidence for the effectiveness of different antioxidants in female subfertility.
Objectives: To determine whether supplementary oral antioxidants compared with placebo, no treatment/standard treatment or another antioxidant improve fertility outcomes for subfertile women.
Search Methods: We searched the following databases (from their inception to September 2016) with no language or date restriction: Cochrane Gynecology and Fertility Group (CGFG) specialized register, the Cochrane Central Register of Studies (CENTRAL CRSO), MEDLINE, Embase, PsycINFO, CINAHL and AMED. We checked reference lists of appropriate studies and searched for ongoing trials in the clinical trials registers.
Selection Criteria: We included randomized controlled trials (RCTs) that compared any type, dose or combination of oral antioxidant supplement with placebo, no treatment or treatment with another antioxidant, among women attending a reproductive clinic. We excluded trials comparing antioxidants with fertility drugs alone and trials that only included fertile women attending a fertility clinic because of male partner infertility.
Data Collection and Analysis: Two review authors independently selected eligible studies, extracted the data and assessed the risk of bias of the included studies. The primary review outcome was live birth; secondary outcomes included clinical pregnancy rates and adverse events. We pooled studies using a fixed-effect model, and calculated odds ratios (ORs) with 95% confidence intervals (CIs) for the dichotomous outcomes of live birth, clinical pregnancy and adverse events. We assessed the overall quality of the evidence by applying GRADE criteria.
Main Results: We included 50 trials involving 6510 women. Investigators compared oral antioxidants, including combinations of antioxidants, N-acetyl-cysteine, melatonin, L-arginine, myo-inositol, D-chiro-inositol, carnitine, selenium, vitamin E, vitamin B complex, vitamin C, vitamin D+calcium, CoQ10, pentoxifylline and omega-3-polyunsaturated fatty acids versus placebo, no treatment/standard treatment or another antioxidant.Very low-quality evidence suggests that antioxidants may be associated with an increased live birth rate compared with placebo or no treatment/standard treatment (OR 2.13, 95% CI 1.45 to 3.12, P > 0.001, 8 RCTs, 651 women, I2 = 47%). This suggests that among subfertile women with an expected live birth rate of 20%, the rate among women using antioxidants would be between 26% and 43%.Very low-quality evidence suggests that antioxidants may be associated with an increased clinical pregnancy rate compared with placebo or no treatment/standard treatment (OR 1.52, 95% CI 1.31 to 1.76, P < 0.001, 26 RCTs, 4271 women, I2 = 66%). This suggests that among subfertile women with an expected clinical pregnancy rate of 22%, the rate among women using antioxidants would be between 27% and 33%. Heterogeneity was moderately high.There was insufficient evidence to determine whether there was a difference between the groups in rates of miscarriage (OR 0.79, 95% CI 0.58 to 1.08, P = 0.14, 18 RCTs, 2834 women, I2 = 23%, very low quality evidence). This suggests that, among subfertile women with an expected miscarriage rate of 7%, use of antioxidants would be expected to result in a miscarriage rate of between 4% and 7%. There was also insufficient evidence to determine whether there was a difference between the groups in rates of multiple pregnancy (OR 1.00, 95% CI 0.73 to 1.38, P = 0.98, 8 RCTs, 2163 women, I2 = 4%, very low quality evidence). This suggests that among subfertile women with an expected multiple pregnancy rate of 8%, use of antioxidants would be expected to result in a multiple pregnancy rate between 6% and 11%. Likewise, there was insufficient evidence to determine whether there was a difference between the groups in rates of gastrointestinal disturbances (OR 1.55, 95% CI 0.47 to 5.10, P = 0.47, 3 RCTs, 343 women, I2 = 0%, very low quality evidence). This suggests that among subfertile women with an expected gastrointestinal disturbance rate of 2%, use of antioxidants would be expected to result in a rate between 1% and 11%. Overall adverse events were reported by 35 trials in the meta-analysis, but there was insufficient evidence to draw any conclusions.Only one trial reported on live birth, clinical pregnancy or adverse effects in the antioxidant versus antioxidant comparison, and no conclusions could be drawn.Very low-quality evidence suggests that pentoxifylline may be associated with an increased clinical pregnancy rate compared with placebo or no treatment (OR 2.07, 95% CI 1.20 to 3.56, P = 0.009, 3 RCTs, 276 women, I2 = 0%). This suggests that among subfertile women with an expected clinical pregnancy rate of 25%, the rate among women using pentoxifylline would be between 28% and 53%.There was insufficient evidence to determine whether there was a difference between the groups in rates of miscarriage (OR 1.34, 95% CI 0.46 to 3.90, P = 0.58, 3 RCTs, 276 women, I2 = 0%) or multiple pregnancy (OR 0.78, 95% CI 0.20 to 3.09, one RCT, 112 women, very low quality evidence). This suggests that among subfertile women with an expected miscarriage rate of 4%, the rate among women using pentoxifylline would be between 2% and 15%. For multiple pregnancy, the data suggest that among subfertile women with an expected multiple pregnancy rate of 9%, the rate among women using pentoxifylline would be between 2% and 23%.The overall quality of evidence was limited by serious risk of bias associated with poor reporting of methods, imprecision and inconsistency.
Author's Conclusions: In this review, there was very low-quality evidence to show that taking an antioxidant may provide benefit for subfertile women, but insufficient evidence to draw any conclusions about adverse events. At this time, there is limited evidence in support of supplemental oral antioxidants for subfertile women.
Fertilichron male Research:
One-carbon cycle support rescues sperm damage in experimentally induced varicocoele in rats.
Mohammadi P1,2, Hassani-Bafrani H2,3, Tavalaee M1, Dattilo M4, Nasr-Esfahani MH1,5.
Abstract:
Objectives: To investigate whether micronutrients in support of the one-carbon cycle and glutathione synthesis are effective in improving sperm damage after surgical varicocoele induction in rats and whether any effect is achieved without a rebound reductive stress as seen with oral antioxidants.
Materials and Methods: Surgical varicocoele was induced in adult male Wistar rats and resulted in significant damage to the testis and sperm cells measured at 2 and 4 months after surgery. At 2 months after surgery, rats received a 2-month oral supplementation in support of the one-carbon cycle containing B vitamins (B2, B3, B6, folic acid and B12), N-acetyl-cysteine, zinc, small amounts of vitamin E, and a natural source of betalains and quercetine (Condensyl® ; Parthenogen SAGL, Lugano, Switzerland and Nurilia SARL, Lyon, France).
Results: One-carbon cycle supplementation, compared to untreated controls, significantly improved the morphometric characteristics of testis (P < 0.05), sperm concentration, motility and abnormal morphology (P < 0.001), sperm chromatin condensation (aniline blue staining, P < 0.05), sperm DNA damage (acridine orange staining, P < 0.05) and sperm lipid peroxidation (BODIPY C11, P < 0.001). The improvement in both nuclear condensation and DNA damage and the lack of excessive inhibition of lipid peroxidation confirmed that no reductive stress had occurred.
Conclusions: Micronutrients in support of the one-carbon cycle are effective in the treatment of surgically induced varicocoele in rats, probably by activating natural antioxidant defences and epigenetics. These results support the idea that essential micronutrients including B vitamins may also have a positive influence in clinical varicocoele, which should be tested in prospective clinical trials.
https://www.ncbi.nlm.nih.gov/pubmed/29752770
Fertilichron female Research:
Can xylene and quercetin directly affect basic ovarian cell functions?
Tarko A1, Štochmalova A2, Hrabovszka S2, Vachanova A2, Harrath AH3, Alwasel S3, Grossman R4, Sirotkin AV5.
Abstract: Exposure to xylene leads to dysfunction of mammalian female reproduction. Quercetin present in vegetables contribute significantly to their role as health-promoting foods. The effects of xylene and quercetin on ovarian cell function, their interrelationships, and mechanisms of action are insufficiently studied. In this in vitro study, we examined the effects of xylene, quercetin, and xylene/quercetin combination on basic bovine ovarian cell functions, such as proliferation, apoptosis, and hormone release. Furthermore, we examined the protective effect of quercetin against the potential negative effects of xylene. Proliferation and apoptosis were assessed via immunocytochemistry using PCNA and BAX markers. The release of progesterone, testosterone, and insulin-like growth factor (IGF-I) was analysed by EIA/RIA. Xylene stimulated proliferation and IGF-I release, but inhibited progesterone and testosterone release. Quercetin inhibited proliferation, apoptosis, and release of IGF-I, progesterone, and testosterone. When administered with xylene, quercetin prevented the action of xylene on proliferation and IGF-I release, induced the stimulatory action of xylene on apoptosis, and promoted the effect of xylene on release of progesterone but not testosterone. These results demonstrated the actions of both xylene and quercetin on basic ovarian cell functions. Furthermore, they show, that quercetin can either prevented or promote xylene effects on the ovarian cells, which indicates potential usefulness of quercetin for prevention of xylene action on female reproduction.
https://www.ncbi.nlm.nih.gov/pubmed/30086515
The effects of quercetin supplementation on metabolic and hormonal parameters as well as plasma concentration and gene expression of resistin in overweight or obese women with polycystic ovary syndrome.
Khorshidi M1, Moini A2,3, Alipoor E4, Rezvan N5, Gorgani-Firuzjaee S6, Yaseri M7, Hosseinzadeh-Attar MJ1,8.
Abstract: The aim of this study was to investigate the effect of quercetin on metabolic and hormonal parameters as well as plasma concentration and gene expression of resistin in overweight or obese women with polycystic ovary syndrome (PCOS). In this randomized, double-blind, placebo-controlled trial, 78 overweight or obese women (25 ≤ BMI ≤ 40 kg/m2 , 20-40 years) with PCOS were recruited. Patients were randomized to receive 1,000 mg/day quercetin or placebo for 12 weeks. Resistin plasma concentration and gene expression in peripheral blood mononuclear cells, parameters of glucose homeostasis, circulatory testosterone, luteinizing hormone (LH), and sex hormone-binding globulin, and anthropometries were assessed at baseline and at the end of the study. Following supplementation, quercetin significantly decreased resistin concentration (2.07 ± 0.23 vs. 2.88 ± 0.40 ng/ml, p < 0.001) and mRNA level (0.64 ± 0.58 vs. 1 ± 0.56 fold change, p = 0.008), compared with placebo group. Moreover, testosterone (0.72 ± 0.15 vs. 0.76 ± 0.12 ng/ml, p = 0.001) and LH (8.05 ± 2.88 vs. 8.77 ± 1.99 mIU/ml, p = 0.035) concentrations were significantly lower in quercetin compared with placebo group. Fasting blood glucose (p < 0.001), insulin (p = 0.02), and homeostatic model assessment of insulin resistance (p = 0.009) decreased within the quercetin group; however, no significant differences were observed compared with the placebo group (p = 0.074, p = 0.226, p = 0.22, respectively). Quercetinsupplementation decreased resistin plasma levels and gene expression, and testosterone and LH concentration in overweight or obese women with PCOS.
https://www.ncbi.nlm.nih.gov/pubmed/30062709
Therapeutic potentials of Quercetin in management of polycystic ovarian syndrome using Letrozole induced rat model: a histological and a biochemical study.
Jahan S1, Abid A1, Khalid S1, Afsar T2, Qurat-Ul-Ain1, Shaheen G1, Almajwal A3, Razak S4,5.
Abstract:
Background: PCOS is a leading endocrinopathy of young women instigating androgens elevation, insulin resistance, obesity, cardiometabolic and menstrual complications. The study investigated the effects of quercetin in a letrozole induced rat model of polycystic ovarian syndrome, which displayed both clinical and metabolic features as in PCOS women.
Methods: Female Sprague Dawley (SD) rats were divided into four groups; control group received aqueous solution of carboxymethyl (CMC 0.5%); PCOS group administered with letrozole (1 mg/kg) dissolved in solution (CMC 0.5%); Metformin group given with metformin (20 mg/kg) + letrozole (1 mg/kg); and Quercetin group provided with quercetin (30 mg/kg) + letrozole (1 mg/kg). All doses were given orally via gavage, for 21 consecutive days and colpocytological analysis was carried till end. After 21rst day, blood was taken out, centrifuged and plasma was kept for biochemical analysis (ELISA, anti-oxidant enzymes, lipid profile) and the reproductive organs were dissected out for histopathological evaluation.
Results: Quercetin as a chief member of flavonoid, showed beneficial effects by decreasing body weight, ovarian diameter, cysts and restoring healthy follicles, follicle's extra-glandular layers, and corpora lutea in contrast to the positive control. Additionally, lipid profile and anti-oxidant status were also maintained to baseline which was very high in diseased rats (p < 0.001).Quercetin depicted a mark regulation in steroidogenesis by decreasing the levels of testosterone (0.78 ng/ml ± 0.14 in quercetin vs. PCOS positive control 1.69 ng/ml ± 0.17, p < 0.001) and estradiol (8.85 pg/ml ± 0.19 in quercetin vs. PCOS positive 1.61 pg/ml ± 0.29) and increasing progesterone levels (34.47 ng/ml ± 1.65 in quercetin vs. 11.08 ng/ml ± 1.17 in PCOS positive). The effects of quercetin were moderately parallel to the standard drug available in market i.e. metformin.
Conclusions: The present study has confirmed that quercetin has the potentials to alleviate the hormonal and metabolic disturbances occurring in PCOS.
https://www.ncbi.nlm.nih.gov/pubmed/29615083
Quercetin supplemented diet improves follicular development, oocyte quality, and reduces ovarian apoptosis in rabbits during summer heat stress.
Naseer Z1, Ahmad E2, Epikmen ET3, Uçan U4, Boyacioğlu M5, İpek E3, Akosy M4.
Abstract: The present study was designed to test the modulatory effect of dietary quercetin on follicle population, apoptosis, in vitro maturation rate and quality of oocytes in heat stressed female rabbits. A total of thirty-four New Zealand White heat stress (HS) exposed female rabbits were either fed with quercetin supplemented diet (QU-HS) or non-supplemented (HS) diet. Firstly, laparotomy was performed for oocyte retrieval and then, oocyte grading and COCs dimensional assessments were conducted. The A and B-grade oocytes were submitted for in vitro maturation. Thereafter, the ovaries were collected from rabbits and were processed for follicular population estimation and granulosa cells apoptosis. The results showed that follicle number, retrieved oocytes and A-grade oocytes were higher in QU-HS, comparatively. A significant difference was observed in A-grade oocytes dimensions between QU-HS and HS treatment groups. The oocyte maturation rate was same across the groups. The quercetin supplementation significantly improved primordial and antral stage follicles. A greater number of apoptotic cells were observed in primary and antral follicles in the HS group. In conclusion, the quercetin provision improves the follicular development, minimize granulosa cells apoptosis, and maintain the oocyte competence in HS rabbits.
Fertilichron male Research:
Wu C, Zhang Y, Shen Q, Zhou Z, Liu W, Hua J.
Oncotarget.2016 Oct 29. doi: 10.18632/oncotarget.12990. [Epub ahead of print]
Resveratrol changes spermatogonial stem cells (SSCs) activity and ameliorates their loss in busulfan-induced infertile mouse.
Abstract: The decline of quantity and quality of sperm are correlated with the increasing age and some anti-cancer compounds such as busulfan. Previous studies have shown that Resveratrol (Res) inhibits tumorigenesis and metastasis of many cancers including mammary tumor, prostate and pancreatic cancers. It acts as anti-age in mouse and human, however, little is known about its protective effect on aged spermatogonial stem cells (SSCs). Here, we investigated the effects of Res in vitro on SSCs usingC18-4 cells and in vivo in busulfan-induced azoospermia mice model. The results showed that Res at different concentrations had different effects on C18-4 cells. Treatment with 2 μM of Res promotes cell proliferation and inhibits apoptosis, but stimulates apoptosis with a higher concentration (20 μM) in C18-4 cells. Using busulfan-induced infertility mice model, we demonstrated that Res (30 mg/kg/d and 100 mg/kg/d) clearly ameliorated SSCs loss to recover the spermatogenesis. Taken together, our data suggest that Res might be an approach for therapeutic intervention to promote SSC proliferation and cease SSCs loss in azoospermia mice model induced by busulfan.
Fertilichron female Research:
Beneficial effect of resveratrol on bovine oocyte maturation and subsequent embryonic development after in vitro fertilization.
Wang F1, Tian X1, Zhang L1, He C1, Ji P1, Li Y1, Tan D2, Liu G3.
Abstract:
Objective: To analyze the potential beneficial effects and mechanisms of action of resveratrol on the maturation of bovine oocytes that were incubated in different concentrations of resveratrol (0.1, 1.0, or 10.0 μM) as germinal vesicle-stage oocytes.
Design: In vitro prospective study.
Setting: University research laboratory.
Animals: Animal models for human studies.
Interventions: In vitro culture in the presence of various concentrations of the antioxidant resveratrol.
Main Outcome Measures: Parameters of hormone levels, oocyte nuclear maturation, cumulus expansion, levels of intracellular glutathione and reactive oxygen species, embryonic cleavage, blastocyst formation, gene expression associated with mature bovine oocytes and cumulus cells, and level of sirtuin 1 gene expression.
Results: Resveratrol statistically significantly increased progesterone secretion and decreased estradiol-17β secretion by cumulus cells. The elevated levels of progesterone activated the Mos/MEK/p42 mitogen-activated protein kinase (MAPK) cascade in the oocytes. At a concentration of 1.0 μM, resveratrol statistically significantly improved cumulus expansion, polar body formation, the (hatched) blastocyst rate, and the mean number of cells/blastocysts. Meanwhile, resveratrol statistically significantly reduced the level of reactive oxygen species (ROS) and increased the level of glutathione (GSH). For the first time, the expression of the sirtuin-1 gene was identified in granulosa cells, cumulus cells, oocytes, and blastocysts. Further studies revealed that resveratrol promoted sirtuin-1 gene expression.
Conclusions: Resveratrol promoted bovine oocyte maturation and subsequent post-in vitro fertilization embryonic development by inducing progesterone secretion and an antioxidant effect, probably in a manner dependent on sirtuin-1.
Copyright © 2014 American Society for Reproductive Medicine. All rights reserved.
https://www.ncbi.nlm.nih.gov/pubmed/24314921
Regulation of SIRT1 determines initial step of endometrial receptivity by controlling E-cadherin expression.
Shirane A1, Wada-Hiraike O, Tanikawa M, Seiki T, Hiraike H, Miyamoto Y, Sone K, Hirano M, Oishi H, Oda K, Kawana K, Nakagawa S, Osuga Y, Fujii T, Yano T, Kozuma S, Taketani Y.
Abstract: Sirtuin 1 (SIRT1), originally found as a class III histone deacetylase, is a principal modulator of pathways downstream of calorie restriction, and the activation of SIRT1 ameliorates glucose homeostasis and insulin sensitivity. We examined the role of SIRT1 in the regulation of uterine receptivity using Ishikawa and RL95-2 endometrial carcinoma cell lines. Exogenous expression of SIRT1 significantly enhanced E-cadherin expression, while small interfering RNA-mediated depletion of endogenous SIRT1 resulted in a significant reduction of E-cadherin expression. A SIRT1 activator resveratrol elevated E-cadherin expression in a dose dependent manner, while SIRT1 repressors nicotinamide and sirtinol exhibited a dose dependent reduction of E-cadherin expression. We also showed that both forced expression of SIRT1 and activation of SIRT1 promote E-cadherin-driven reporter gene constructs, and SIRT1 is localized at E-cadherin promoter containing E-box elements in Ishikawa cells. Using an in vitro model of embryo implantation, we demonstrate that exogenous expression of SIRT1 and stimulation of SIRT1 activity resulted in the Ishikawa cell line becoming receptive to JAR cell spheroid attachment. Furthermore, resveratrol enhanced E-cadherin and Glycodelin protein expression at sites of intercellular contact, suggesting an additive role of resveratrol in promoting implantation. The initial step of human reproduction depends on the capacity of an embryo to attach and implant into the endometrial wall, and these results revealed the novel mechanism that activation and increased expression of SIRT1 play an important role in uterine receptivity.
Fertilichron male Research:
Effects of xinxibao (Zinc plus Selene) on sperm quality in oligoasthenozoospermic men (n=34, open trail per 3 month).
Shi Yet al., Zhonghua Nan Ke Xue 2004
Abstract:
Objective: To evaluate the effects of zinc and selenium on the sperm quality of oligoasthenozoospermic men.
Methods: Thirty-four cases of oligoasthenozoospermia were treated with Xinxibao (Zinc & Selenium Tablet) three times a day and five tablets at a time for ninety days in succession. The seminal routine analysis was performed by computer-assisted sperm analysis (CASA) at the end of each month. RESULTS: The sperm quality was improved significantly sixty days and ninety days after treatment. Five cases (14.7%) showed remarkable effect, 25 (73.5%) improved, and 4 (11.8%) did not respond.
Conclusion: Zinc and selenium can significantly improve the sperm quality of oligoasthenozoospermic men.
A post-publication analysis of the idealized upper reference value of 2.5 mIU/L for TSH: Time to support the thyroid axis with magnesium and iron especially in the setting of reproduction medicine.
Abstract: Laboratory medicine approaches the evaluation of thyroid function mostly through the single determination of the blood level of thyroid stimulating hormone (TSH). Some authors have suggested an upper reference value for TSH of 2.5 mIU/L. This suggestion has not been confirmed by recent clinical studies. These studies have delivered a clinically valid reference range going from 0.3 to 3.5 mIU/L. These values are valid for both for the general population as well as in the setting of fertility and pregnancy. Current biochemical evidence about the elements required to maintain thyroid function shows that these not only include dietary iodine but also magnesium, iron, selenium and coenzyme Q10. Iron is important for the synthesis of thyroid peroxidase; magnesium-ATP contributes to the active process of iodine uptake; iodine has to be sufficiently present in the diet; selenium acts through selenoproteins to protect the thyroid cell during hormone synthesis and in deiodination of thyroxine; coenzyme Q10 influences thyroid vascularity. As a consequence, good clinical practice requires additional biochemical information on the blood levels of magnesium, selenium, coenzyme Q10 as well as iron status. Since these elements are also important for the maintenance of reproductive function, we postulate that they constitute the connecting link between both endocrine systems.
https://www.ncbi.nlm.nih.gov/pubmed/28409122
Lipovac M, Bodner F, Imhof M, Chedraui P.
Reprod Biol Endocrinol.2016 Dec 9;14(1):84.
Comparison of the effect of a combination of eight micronutrients versus a standard mono preparation on sperm parameters.
Abstract:
Background: There are reports showing that l-carnitine alone or in combination with other micronutrients improve sperm parameters. However, comparative studies are still lacking. This study was carried out to compare the short term effects of a combination of eight micronutrients including l-carnitine vs. a mono-substance (l-carnitine alone) on sperm parameters.
Methods: This was a prospective, open-labelled, nonrandomized study that included male subjects (20 to 60 years) with at least 1 year of subfertility and at least one pathological semen analysis who received 3 months treatment with a mono-substance (500 mg l-carnitine/twice a day, n = 156) or a combined compound (440 mg l-carnitine + 250 mg l-arginine + 40 mg zinc + 120 mg vitamin E + 80 mg glutathione + 60 μg selenium + 15 mg coenzyme Q10 + 800 μg folic acid/once a day, n = 143) for the same time period. Sperm parameters were analyzed before and after treatment and groups comparisons performed.
Results: Baseline characteristics were similar among studied groups (age and body mass indices). Semen parameters (volume, density, overall progressive motility [including slow and fast motility]) and percentage of sperm with normal morphology improved after 3 months in both groups as compared to baseline. However, relative change (expressed as % increase of absolute values) for sperm density and overall progressive motility (including fast motility) was found to be higher for the combined micronutrient treatment group as compared to the mono-treatment using l-carnitine alone.
Conclusion: Both analyzed groups displayed a positive short term effect on all sperm parameters; however effect on density and motility was significantly better for the combined formulation. There is need for more research in this matter that includes long term outcome data.
Fertilichron female Research:
Micronutrition and fertility problems in women: What is essential?
Article · April 2017 with 3 Reads
Abstract: New way of life of modern women (tobacco, alcohol, polluted environment, industrial food, endocrine disruptor, etc.) causes an increase of production of reactive oxygen species that affect female fertility. It was found that oxidative stress may damage the oocytes and may impair their fertilization capacity. The aim of this review of recent studies is to select natural ingredients able to reduce oxidative stress. A combination of vitamins (B, C and E), minerals (selenium, iodine) and myo-inositol could be useful as an alternative way, on top of balanced diet and lifestyle advice, for women planning to become pregnant including those with or without SOPK.
Micronutrition and fertility problems in women: What is essential?. Available from: https://www.researchgate.net/publication/319078771_Micronutrition_and_fertility_problems_in_women_What_is_essential?ev=publicSearchHeader&_sg=OLkflgbUBKR-DW8BnuhjARU6gATKsqVmAZziZwYqFsGhEAPbuv8Sktg1NM4DT_khpyLjwXNZ0JcnnAw
The effect of micronutrient supplements on female fertility.
Abstract:
Purpose of Review: Benefit of micronutrient supplementation on female fertility.
Recent Findings: Reports of randomized trials are rare. Most studies are focused on multivitamin supplementations. For some micronutrients, a positive impact on fertility could be shown. This article reviews the available clinical studies as well as the pathophysiological background of possible effects and summarizes the potential benefits of selected micronutrients on female fertility.
Summary: Apart from lowering the malformation risk by periconceptional supplementation of folic acid, substitution with different micronutrients, particularly folic acid, vitamin B6, vitamin C, vitamin D, vitamin E, iodine, selenium, iron, and DHA might have a positive impact on infertility treatment. The multivitamin formulation should take the pathophysiology, clinical studies, and upper limits into account.
https://www.ncbi.nlm.nih.gov/pubmed/23571830
Antioxidants for female subfertility.
Showell MG1, Mackenzie-Proctor R, Jordan V, Hart RJ.
Abstract:
Background: A couple may be considered to have fertility problems if they have been trying to conceive for over a year with no success. This may affect up to a quarter of all couples planning a child. It is estimated that for 40% to 50% of couples, subfertility may result from factors affecting women. Antioxidants are thought to reduce the oxidative stress brought on by these conditions. Currently, limited evidence suggests that antioxidants improve fertility, and trials have explored this area with varied results. This review assesses the evidence for the effectiveness of different antioxidants in female subfertility.
Objectives: To determine whether supplementary oral antioxidants compared with placebo, no treatment/standard treatment or another antioxidant improve fertility outcomes for subfertile women.
Search Methods: We searched the following databases (from their inception to September 2016) with no language or date restriction: Cochrane Gynecology and Fertility Group (CGFG) specialized register, the Cochrane Central Register of Studies (CENTRAL CRSO), MEDLINE, Embase, PsycINFO, CINAHL and AMED. We checked reference lists of appropriate studies and searched for ongoing trials in the clinical trials registers.
Selection Criteria: We included randomized controlled trials (RCTs) that compared any type, dose or combination of oral antioxidant supplement with placebo, no treatment or treatment with another antioxidant, among women attending a reproductive clinic. We excluded trials comparing antioxidants with fertility drugs alone and trials that only included fertile women attending a fertility clinic because of male partner infertility.
Data Collection and Analysis: Two review authors independently selected eligible studies, extracted the data and assessed the risk of bias of the included studies. The primary review outcome was live birth; secondary outcomes included clinical pregnancy rates and adverse events. We pooled studies using a fixed-effect model, and calculated odds ratios (ORs) with 95% confidence intervals (CIs) for the dichotomous outcomes of live birth, clinical pregnancy and adverse events. We assessed the overall quality of the evidence by applying GRADE criteria.
Main Results: We included 50 trials involving 6510 women. Investigators compared oral antioxidants, including combinations of antioxidants, N-acetyl-cysteine, melatonin, L-arginine, myo-inositol, D-chiro-inositol, carnitine, selenium, vitamin E, vitamin B complex, vitamin C, vitamin D+calcium, CoQ10, pentoxifylline and omega-3-polyunsaturated fatty acids versus placebo, no treatment/standard treatment or another antioxidant.Very low-quality evidence suggests that antioxidants may be associated with an increased live birth rate compared with placebo or no treatment/standard treatment (OR 2.13, 95% CI 1.45 to 3.12, P > 0.001, 8 RCTs, 651 women, I2 = 47%). This suggests that among subfertile women with an expected live birth rate of 20%, the rate among women using antioxidants would be between 26% and 43%.Very low-quality evidence suggests that antioxidants may be associated with an increased clinical pregnancy rate compared with placebo or no treatment/standard treatment (OR 1.52, 95% CI 1.31 to 1.76, P < 0.001, 26 RCTs, 4271 women, I2 = 66%). This suggests that among subfertile women with an expected clinical pregnancy rate of 22%, the rate among women using antioxidants would be between 27% and 33%. Heterogeneity was moderately high.There was insufficient evidence to determine whether there was a difference between the groups in rates of miscarriage (OR 0.79, 95% CI 0.58 to 1.08, P = 0.14, 18 RCTs, 2834 women, I2 = 23%, very low quality evidence). This suggests that, among subfertile women with an expected miscarriage rate of 7%, use of antioxidants would be expected to result in a miscarriage rate of between 4% and 7%. There was also insufficient evidence to determine whether there was a difference between the groups in rates of multiple pregnancy (OR 1.00, 95% CI 0.73 to 1.38, P = 0.98, 8 RCTs, 2163 women, I2 = 4%, very low quality evidence). This suggests that among subfertile women with an expected multiple pregnancy rate of 8%, use of antioxidants would be expected to result in a multiple pregnancy rate between 6% and 11%. Likewise, there was insufficient evidence to determine whether there was a difference between the groups in rates of gastrointestinal disturbances (OR 1.55, 95% CI 0.47 to 5.10, P = 0.47, 3 RCTs, 343 women, I2 = 0%, very low quality evidence). This suggests that among subfertile women with an expected gastrointestinal disturbance rate of 2%, use of antioxidants would be expected to result in a rate between 1% and 11%. Overall adverse events were reported by 35 trials in the meta-analysis, but there was insufficient evidence to draw any conclusions.Only one trial reported on live birth, clinical pregnancy or adverse effects in the antioxidant versus antioxidant comparison, and no conclusions could be drawn.Very low-quality evidence suggests that pentoxifylline may be associated with an increased clinical pregnancy rate compared with placebo or no treatment (OR 2.07, 95% CI 1.20 to 3.56, P = 0.009, 3 RCTs, 276 women, I2 = 0%). This suggests that among subfertile women with an expected clinical pregnancy rate of 25%, the rate among women using pentoxifylline would be between 28% and 53%.There was insufficient evidence to determine whether there was a difference between the groups in rates of miscarriage (OR 1.34, 95% CI 0.46 to 3.90, P = 0.58, 3 RCTs, 276 women, I2 = 0%) or multiple pregnancy (OR 0.78, 95% CI 0.20 to 3.09, one RCT, 112 women, very low quality evidence). This suggests that among subfertile women with an expected miscarriage rate of 4%, the rate among women using pentoxifylline would be between 2% and 15%. For multiple pregnancy, the data suggest that among subfertile women with an expected multiple pregnancy rate of 9%, the rate among women using pentoxifylline would be between 2% and 23%.The overall quality of evidence was limited by serious risk of bias associated with poor reporting of methods, imprecision and inconsistency.
Authors' Conclusions: In this review, there was very low-quality evidence to show that taking an antioxidant may provide benefit for subfertile women, but insufficient evidence to draw any conclusions about adverse events. At this time, there is limited evidence in support of supplemental oral antioxidants for subfertile women.
https://www.ncbi.nlm.nih.gov/pubmed/28752910
A post-publication analysis of the idealized upper reference value of 2.5 mIU/L for TSH: Time to support the thyroid axis with magnesium and iron especially in the setting of reproduction medicine.
Abstract:
Laboratory medicine approaches the evaluation of thyroid function mostly through the single determination of the blood level of thyroid stimulating hormone (TSH). Some authors have suggested an upper reference value for TSH of 2.5 mIU/L. This suggestion has not been confirmed by recent clinical studies. These studies have delivered a clinically valid reference range going from 0.3 to 3.5 mIU/L. These values are valid for both for the general population as well as in the setting of fertility and pregnancy. Current biochemical evidence about the elements required to maintain thyroid function shows that these not only include dietary iodine but also magnesium, iron, selenium and coenzyme Q10. Iron is important for the synthesis of thyroid peroxidase; magnesium-ATP contributes to the active process of iodine uptake; iodine has to be sufficiently present in the diet; selenium acts through selenoproteins to protect the thyroid cell during hormone synthesis and in deiodination of thyroxine; coenzyme Q10 influences thyroid vascularity. As a consequence, good clinical practice requires additional biochemical information on the blood levels of magnesium, selenium, coenzyme Q10 as well as iron status. Since these elements are also important for the maintenance of reproductive function, we postulate that they constitute the connecting link between both endocrine systems.
Fertilichron male Research:
Antioxidants and Phytocompounds on Seminal Oxidative Stress
Article (PDF Available) · March 2017 with 184 Reads
DOI: 10.3390/diseases5010009
Abstract: Defective sperm function has been identified as the most common cause of infertility. The objective of this study was to review recent findings on the effects of various antioxidants on male fertility. High amounts of poly unsaturated fatty acid are found in the mammalian spermatozoa membranes, thereby making them susceptible to lipid peroxidation. Although, free radicals and reactive oxygen species (ROS) play major roles in reproduction, they are strongly associated with oxidative stress. Furthermore, factors such as obesity, inflammation, pollutants and cigarette smoking are negatively correlated with spermatogenesis. Endogenous antioxidants system exists to mediate these damages. In a normal physiological state, the seminal plasma contains antioxidant enzyme mechanism that is capable of quenching these ROS as well as protecting the spermatozoa against any likely damage. However, high level of ROS triggered by inflammatory cells and oxidation of fatty acid in obese subjects may down play antioxidant mechanism resulting in oxidative stress. Evaluation of such oxidative stress is the first step in the treatment of male infertility through administration of suitable antioxidant. Notably, antioxidant such as vitamin E and C, carotenoids and carnitine have been found beneficial in restoring a balance between ROS generation and scavenging activities. There are emerging evidences that herbal products can also boost male reproductive functions. Nonetheless, a good lifestyle, regular exercise, avoidance of stress and observing safety rules at work are habits that can reverse male infertility.
(PDF) Male Infertility: The Effect of Natural Antioxidants and Phytocompounds on Seminal Oxidative Stress. Available from: https://www.researchgate.net/publication/314202739_Male_Infertility_The_Effect_of_Natural_Antioxidants_and_Phytocompounds_on_Seminal_Oxidative_Stress
Dietary patterns, foods and nutrients in male fertility parameters and fecundability: a systematic review of observational studies.
Salas-Huetos A1,2, Bulló M1,2, Salas-Salvadó J1,2.
Abstract:
Background: Infertility is a global public health issue, affecting 15% of all couples of reproductive age. Male factors, including decreased semen quality, are responsible for ~25% of these cases. The dietary pattern, the components of the diet and nutrients have been studied as possible determinants of sperm function and/or fertility.
Objective and Rationale: Previous systematic reviews have been made of the few heterogeneous low-quality randomized clinical trials (RCTs) conducted in small samples of participants and investigating the effect of specific nutrients and nutritional supplements on male infertility. However, as yet there has been no systematic review of observational studies.
Search Methods: A comprehensive systematic review was made of the published literature, from the earliest available online indexing year to November 2016, in accordance with the guidelines of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses. We have included cross-sectional, case-control and prospective and retrospective studies in which fertile/infertile men were well defined (men with sperm disorders, sperm DNA damage, varicocele or idiopathic infertility). The primary outcomes were semen quality or fecundability. With the data extracted, we evaluated and scored the quality of the studies selected. We excluded RCTs, animal studies, review articles and low-quality studies.
Outcomes: A total of 1944 articles were identified, of which 35 were selected for qualitative analysis. Generally, the results indicated that healthy diets rich in some nutrients such as omega-3 fatty acids, some antioxidants (vitamin E, vitamin C, β-carotene, selenium, zinc, cryptoxanthin and lycopene), other vitamins (vitamin D and folate) and low in saturated fatty acids and trans-fatty acids were inversely associated with low semen quality parameters. Fish, shellfish and seafood, poultry, cereals, vegetables and fruits, low-fat dairy and skimmed milk were positively associated with several sperm quality parameters. However, diets rich in processed meat, soy foods, potatoes, full-fat dairy and total dairy products, cheese, coffee, alcohol, sugar-sweetened beverages and sweets have been detrimentally associated with the quality of semen in some studies. As far as fecundability is concerned, a high intake of alcohol, caffeine and red meat and processed meat by males has a negative influence on the chance of pregnancy or fertilization rates in their partners.
Wider Implications: Male adherence to a healthy diet could improve semen quality and fecundability rates. Since observational studies may prove associations but not causation, the associations summarized in the present review need to be confirmed with large prospective cohort studies and especially with well-designed RCTs.
https://www.ncbi.nlm.nih.gov/pubmed/28333357
Fertilichron female Research:
Female dietary antioxidant intake and time to pregnancy among couples treated for unexplained infertility.
Ruder EH1, Hartman TJ2, Reindollar RH3, Goldman MB4.
Abstract:
Objective: To determine whether increased antioxidant intake in women is associated with shorter time to pregnancy (TTP) among a cohort of couples being treated for unexplained infertility.
Design: Secondary data analysis of a randomized controlled trial.
Setting: Academic medical center associated with a private infertility center.
Patients: Females with unexplained infertility.
Interventions: None.
Main Outcome Measures: The time it took to establish a pregnancy that led to a live birth.
Results: Mean nutrient intake exceeded the estimated average requirement (EAR) for vitamins C and E. No differences in mean intake of any of the antioxidants were noted between women who delivered a live-born infant during the study period vs. those who did not. In multivariable models, intake of β-carotene from dietary supplements was associated with shorter TTP among women with body mass index (BMI) ≥25 kg/m(2) (hazard ratio [HR] 1.29, 95% confidence interval [CI] 1.09-1.53) and women <35 y (HR 1.19, 95% CI 1.01-1.41). Intake of vitamin C from dietary supplements was associated with shorter TTP among women with BMI <25 kg/m(2) (HR 1.09, 95% CI 1.03-1.15) and women <35 y (HR 1.10, 95% CI 1.02-1.18). Intake of vitamin E from dietary supplements among women ≥35 y also was associated with shorter TTP (HR 1.07, 95% CI 1.01-1.13).
Conclusions: Shorter TTP was observed among women with BMI <25 kg/m(2) with increasing vitamin C, women with BMI ≥25 kg/m(2) with increasing β-carotene, women <35 y with increasing β-carotene and vitamin C, and women ≥35 y with increasing vitamin E.
CLINICAL TRIAL REGISTRATION NUMBER:
Fertilichron male Research:
J Nutr Sci Vitaminol (Tokyo).2012;58(4):230-9.
The interactive effect of dietary water-soluble vitamin levels on the depression of gonadal development in growing male rats kept under disturbed daily rhythm.
Abstract: The purpose of this study was to clarify the effects of nutrients on the gonadal development of male rats kept under constant darkness as a model of disturbed daily rhythm. In the present study we examined the effects of nine water-soluble vitamins. We selected 7 water-soluble vitamins (choline, nicotinic acid (NA), pantothenic acid (PA), vitamin B6 (VB6), vitamin B1 (VB1), vitamin B2 (VB2) and folic acid (FA)) as experimental factors for the first experiment (Ex. 1) and biotin and vitamin B12 (VB12) as experimental factors for the second experiment (Ex. 2). The dietary content of these vitamins was normal or six times the normal content. Lighting condition (L.C.) was also added as a factor. Four-week-old male rats (Fischer 344 strain) were kept under constant darkness or normal lighting (12-h light/dark cycle) for 4 wk. The depression of gonadal development in the constant darkness groups (D-groups) was shown. The L.C., PA, VB6 and VB1 influenced testes development, and these three vitamins had interactions with L.C. Among the normal lighting groups (N-groups), the highest value for testes weight was observed under the normal-PA, high-VB6 and high-B1 diet; on the other hand, among the D-groups, it was observed under the high-PA, normal-VB6 and normal-VB1 diet. The results showed that the depression of gonadal development in rats kept under disturbed daily rhythm was improved by getting a high amount of PA and normal amount of VB6 and VB1.
Fertilichron male Research:
One-carbon cycle support rescues sperm damage in experimentally induced varicocoele in rats.
Mohammadi P1,2, Hassani-Bafrani H2,3, Tavalaee M1, Dattilo M4, Nasr-Esfahani MH1,5.
Abstract:
Objectives: To investigate whether micronutrients in support of the one-carbon cycle and glutathione synthesis are effective in improving sperm damage after surgical varicocele induction in rats and whether any effect is achieved without a rebound reductive stress as seen with oral antioxidants.
Materials and Methods: Surgical varicocele was induced in adult male Wistar rats and resulted in significant damage to the testis and sperm cells measured at 2 and 4 months after surgery. At 2 months after surgery, rats received a 2-month oral supplementation in support of the one-carbon cycle containing B vitamins (B2, B3, B6, folic acid and B12), N-acetyl-cysteine, zinc, small amounts of vitamin E, and a natural source of betalains and quercetine (Condensyl® ; Parthenogen SAGL, Lugano, Switzerland and Nurilia SARL, Lyon, France).
Results: One-carbon cycle supplementation, compared to untreated controls, significantly improved the morphometric characteristics of testis (P < 0.05), sperm concentration, motility and abnormal morphology (P < 0.001), sperm chromatin condensation (aniline blue staining, P < 0.05), sperm DNA damage (acridine orange staining, P < 0.05) and sperm lipid peroxidation (BODIPY C11, P < 0.001). The improvement in both nuclear condensation and DNA damage and the lack of excessive inhibition of lipid peroxidation confirmed that no reductive stress had occurred.
Conclusions: Micronutrients in support of the one-carbon cycle are effective in the treatment of surgically induced varicocele in rats, probably by activating natural antioxidant defenses and epigenetics. These results support the idea that essential micronutrients including B vitamins may also have a positive influence in clinical varicocoele, which should be tested in prospective clinical trials.
Fertilichron male Research:
One-carbon cycle support rescues sperm damage in experimentally induced varicocoele in rats.
Mohammadi P1,2, Hassani-Bafrani H2,3, Tavalaee M1, Dattilo M4, Nasr-Esfahani MH1,5.
Abstract:
Objectives: To investigate whether micronutrients in support of the one-carbon cycle and glutathione synthesis are effective in improving sperm damage after surgical varicocele induction in rats and whether any effect is achieved without a rebound reductive stress as seen with oral antioxidants.
Materials and Methods: Surgical varicocele was induced in adult male Wistar rats and resulted in significant damage to the testis and sperm cells measured at 2 and 4 months after surgery. At 2 months after surgery, rats received a 2-month oral supplementation in support of the one-carbon cycle containing B vitamins (B2, B3, B6, folic acid and B12), N-acetyl-cysteine, zinc, small amounts of vitamin E, and a natural source of betalains and quercetine (Condensyl® ; Parthenogen SAGL, Lugano, Switzerland and Nurilia SARL, Lyon, France).
Results: One-carbon cycle supplementation, compared to untreated controls, significantly improved the morphometric characteristics of testis (P < 0.05), sperm concentration, motility and abnormal morphology (P < 0.001), sperm chromatin condensation (aniline blue staining, P < 0.05), sperm DNA damage (acridine orange staining, P < 0.05) and sperm lipid peroxidation (BODIPY C11, P < 0.001). The improvement in both nuclear condensation and DNA damage and the lack of excessive inhibition of lipid peroxidation confirmed that no reductive stress had occurred.
Conclusions: Micronutrients in support of the one-carbon cycle are effective in the treatment of surgically induced varicocele in rats, probably by activating natural antioxidant defenses and epigenetics. These results support the idea that essential micronutrients including B vitamins may also have a positive influence in clinical varicocoele, which should be tested in prospective clinical trials.
Fertilichron male Research:
J Nutr Sci Vitaminol (Tokyo).2012;58(4):230-9.
The interactive effect of dietary water-soluble vitamin levels on the depression of gonadal development in growing male rats kept under disturbed daily rhythm.
Abstract: The purpose of this study was to clarify the effects of nutrients on the gonadal development of male rats kept under constant darkness as a model of disturbed daily rhythm. In the present study we examined the effects of nine water-soluble vitamins. We selected 7 water-soluble vitamins (choline, nicotinic acid (NA), pantothenic acid (PA), vitamin B6 (VB6), vitamin B1 (VB1), vitamin B2 (VB2) and folic acid (FA)) as experimental factors for the first experiment (Ex. 1) and biotin and vitamin B12 (VB12) as experimental factors for the second experiment (Ex. 2). The dietary content of these vitamins was normal or six times the normal content. Lighting condition (L.C.) was also added as a factor. Four-week-old male rats (Fischer 344 strain) were kept under constant darkness or normal lighting (12-h light/dark cycle) for 4 wk. The depression of gonadal development in the constant darkness groups (D-groups) was shown. The L.C., PA, VB6 and VB1 influenced testes development, and these three vitamins had interactions with L.C. Among the normal lighting groups (N-groups), the highest value for testes weight was observed under the normal-PA, high-VB6 and high-B1 diet; on the other hand, among the D-groups, it was observed under the high-PA, normal-VB6 and normal-VB1 diet. The results showed that the depression of gonadal development in rats kept under disturbed daily rhythm was improved by getting a high amount of PA and normal amount of VB6 and VB1.
Fertilichron male Research:
One-carbon cycle support rescues sperm damage in experimentally induced varicocele in rats.
Mohammadi P1,2, Hassani-Bafrani H2,3, Tavalaee M1, Dattilo M4, Nasr-Esfahani MH1,5.
Abstract:
Objective: To investigate whether micronutrients in support of the one-carbon cycle and glutathione synthesis are effective in improving sperm damage after surgical varicocele induction in rats and whether any effect is achieved without a rebound reductive stress as seen with oral antioxidants.
Materials and Methods: Surgical varicocele was induced in adult male Wistar rats and resulted in significant damage to the testis and sperm cells measured at 2 and 4 months after surgery. At 2 months after surgery, rats received a 2-month oral supplementation in support of the one-carbon cycle containing B vitamins (B2, B3, B6, folic acid and B12), N-acetyl-cysteine, zinc, small amounts of vitamin E, and a natural source of betalains and quercetine (Condensyl® ; Parthenogen SAGL, Lugano, Switzerland and Nurilia SARL, Lyon, France).
Results: One-carbon cycle supplementation, compared to untreated controls, significantly improved the morphometric characteristics of testis (P < 0.05), sperm concentration, motility and abnormal morphology (P < 0.001), sperm chromatin condensation (aniline blue staining, P < 0.05), sperm DNA damage (acridine orange staining, P < 0.05) and sperm lipid peroxidation (BODIPY C11, P < 0.001). The improvement in both nuclear condensation and DNA damage and the lack of excessive inhibition of lipid peroxidation confirmed that no reductive stress had occurred.
Conclusions: Micronutrients in support of the one-carbon cycle are effective in the treatment of surgically induced varicocele in rats, probably by activating natural antioxidant defenses and epigenetics. These results support the idea that essential micronutrients including B vitamins may also have a positive influence in clinical varicocoele, which should be tested in prospective clinical trials.
https://www.ncbi.nlm.nih.gov/pubmed/29752770
J Nutr Sci Vitaminol (Tokyo).2012;58(4):230-9.
The interactive effect of dietary water-soluble vitamin levels on the depression of gonadal development in growing male rats kept under disturbed daily rhythm.
Abstract: The purpose of this study was to clarify the effects of nutrients on the gonadal development of male rats kept under constant darkness as a model of disturbed daily rhythm. In the present study we examined the effects of nine water-soluble vitamins. We selected 7 water-soluble vitamins (choline, nicotinic acid (NA), pantothenic acid (PA), vitamin B6 (VB6), vitamin B1 (VB1), vitamin B2 (VB2) and folic acid (FA)) as experimental factors for the first experiment (Ex. 1) and biotin and vitamin B12 (VB12) as experimental factors for the second experiment (Ex. 2). The dietary content of these vitamins was normal or six times the normal content. Lighting condition (L.C.) was also added as a factor. Four-week-old male rats (Fischer 344 strain) were kept under constant darkness or normal lighting (12-h light/dark cycle) for 4 wk. The depression of gonadal development in the constant darkness groups (D-groups) was shown. The L.C., PA, VB6 and VB1 influenced testes development, and these three vitamins had interactions with L.C. Among the normal lighting groups (N-groups), the highest value for testes weight was observed under the normal-PA, high-VB6 and high-B1 diet; on the other hand, among the D-groups, it was observed under the high-PA, normal-VB6 and normal-VB1 diet. The results showed that the depression of gonadal development in rats kept under disturbed daily rhythm was improved by getting a high amount of PA and normal amount of VB6 and VB1.
Fertilichron female Research:
The effect of micronutrient supplements on female fertility.
Abstract:
Purpose of Review: Benefit of micronutrient supplementation on female fertility.
Recent Findings: Reports of randomized trials are rare. Most studies are focused on multivitamin supplementations. For some micronutrients, a positive impact on fertility could be shown. This article reviews the available clinical studies as well as the pathophysiological background of possible effects and summarizes the potential benefits of selected micronutrients on female fertility.
Summary: Apart from lowering the malformation risk by periconceptional supplementation of folic acid, substitution with different micronutrients, particularly folic acid, vitamin B6, vitamin C, vitamin D, vitamin E, iodine, selenium, iron, and DHA might have a positive impact on infertility treatment. The multivitamin formulation should take the pathophysiology, clinical studies, and upper limits into account.
https://www.ncbi.nlm.nih.gov/pubmed/23571830
The effect of micronutrient supplements on female fertility: a systematic review.
Grajecki D1, Zyriax BC, Buhling KJ.
Abstract:
Purpose: Assessment of the influence of vitamins, trace elements and multivitamin supplements on female fertility.
Methods: Systematic review of published controlled trials and cohort studies investigating the effect of vitamin supplements on female fertility. 13 studies with a total of 90,004 female test persons and patients.
Inclusion Criteria: oral, preconceptional administration of single or combination of vitamin supplements;
Exclusion Criteria: experimental studies, pharmacological studies, case control studies, case reports, reviews, meta-analysis. Women with chronic diseases, genetic or physical causes for (primary) sterility, couples with an impaired fertility of both partners; patients undergoing reproductive medicine care (insemination, in vitro fertilization, IVF, intracytoplasmatic sperm injection, ICSI). Determination of the proportion of women that experienced an influence of vitamin supplements on their fertility.
Results: Thirteen relevant trials out of 37 studies were included. Some studies suggest a possible effect of micronutrients on female fertility. Emphasized results, for example, were an association between multivitamin substitution on pregnancy rate as well as higher vitamin B6 levels in fertile women compared to infertile women. One randomised controlled study showed a positive effect of vitamin C in women with luteal insufficiency.
Conclusion: Although some studies suggest possible effects of micronutrients on female fertility general recommendations are not possible since all studies had methodological or statistical limitations. Further investigations using evidence-based criteria are necessary to analyze and to confirm these non-evident appearances.
Fertilichron male Research:
One-carbon cycle support rescues sperm damage in experimentally induced varicocoele in rats.
Mohammadi P1,2, Hassani-Bafrani H2,3, Tavalaee M1, Dattilo M4, Nasr-Esfahani MH1,5.
Abstract:
Objectives: To investigate whether micronutrients in support of the one-carbon cycle and glutathione synthesis are effective in improving sperm damage after surgical varicocele induction in rats and whether any effect is achieved without a rebound reductive stress as seen with oral antioxidants.
Materials and Methods: Surgical varicocele was induced in adult male wistar rats and resulted in significant damage to the testis and sperm cells measured at 2 and 4 months after surgery. At 2 months after surgery, rats received a 2-month oral supplementation in support of the one-carbon cycle containing b vitamins (b2, b3, b6, folic acid and b12), n-acetyl-cysteine, zinc, small amounts of vitamin e, and a natural source of betalains and quercetine (condensyl® ; parthenogen sagl, lugano, switzerland and nurilia sarl, lyon, france).
Results: One-carbon cycle supplementation, compared to untreated controls, significantly improved the morphometric characteristics of testis (p < 0.05), sperm concentration, motility and abnormal morphology (p < 0.001), sperm chromatin condensation (aniline blue staining, p < 0.05), sperm DNA damage (acridine orange staining, p < 0.05) and sperm lipid peroxidation (bodipy c11, p < 0.001). The improvement in both nuclear condensation and dna damage and the lack of excessive inhibition of lipid peroxidation confirmed that no reductive stress had occurred.
Conclusions: Micronutrients in support of the one-carbon cycle are effective in the treatment of surgically induced varicocele in rats, probably by activating natural antioxidant defenses and epigenetics. These results support the idea that essential micronutrients including B vitamins may also have a positive influence in clinical varicocele, which should be tested in prospective clinical trials.
Https://www.ncbi.nlm.nih.gov/pubmed/29752770
Fertilichron female Research:
A combined supplementation of omega-3 fatty acids and micronutrients (folic acid, vitamin B12) reduces oxidative stress markers in a rat model of pregnancy induced hypertension.
Kemse NG1, Kale AA1, Joshi SR1.
Abstract:
Objectives: Our earlier studies have highlighted that an altered one carbon metabolism (vitamin b12, folic acid, and docosahexaenoic acid) is associated with preeclampsia. Preeclampsia is also known to be associated with oxidative stress and inflammation. The current study examines whether maternal folic acid, vitamin b12 and omega-3 fatty acid supplementation given either individually or in combination can ameliorate the oxidative stress markers in a rat model of pregnancy induced hypertension (pih).
Materials and Methods: Pregnant wistar rats were assigned to control and five treatment groups: pih; pih + vitamin b12; pih + folic acid; pih + omega-3 fatty acids and pih + combined micronutrient supplementation (vitamin b12 + folic acid + omega-3 fatty acids). L-nitroarginine methylester (l-name; 50 mg/kg body weight/day) was used to induce hypertension during pregnancy. Blood pressure (bp) was recorded during pregnancy and dams were dissected at d20 of gestation.
Results: Animals from the PIH group demonstrated higher (p<0.01 for both) systolic and diastolic BP; lower (p<0.01) pup weight; higher dam plasma homocysteine (p<0.05) and dam and offspring malondialdehyde (MDA) (p<0.01), lower (p<0.05) placental and offspring liver DHA and higher (p<0.01) tumor necrosis factor-alpha (TNF-ά) levels as compared to control. Individual micronutrient supplementation did not offer much benefit. In contrast, combined supplementation lowered systolic BP, homocysteine, MDA and placental TNF-ά levels in dams and liver MDA and protein carbonyl in the offspring as compared to PIH group.
Conclusion: Key constituents of one carbon cycle (folic acid, vitamin B12 and DHA) may play a role in reducing oxidative stress and inflammation in preeclampsia.
https://www.ncbi.nlm.nih.gov/pubmed/25405347
The periconceptional period, reproduction and long-term health of offspring: the importance of one-carbon metabolism.
Steegers-Theunissen RP1, Twigt J, Pestinger V, Sinclair KD.
Abstract:
Background: Most reproductive failures originate during the periconceptional period and are influenced by the age and the lifestyle of parents-to-be. We advance the hypothesis that these failures can arise as a partial consequence of derangements to one-carbon (1-C) metabolism (i.e. metabolic pathways that utilize substrates/cofactors such as methionine, vitamin B12, folate). 1-C metabolic pathways drive the synthesis of proteins, biogenic amines and lipids required for early growth, together with the synthesis and methylation of DNA and histones essential for the regulation of gene expression. We review how deficiencies in periconceptional 1-C metabolism affect fertility and development together with underlying mechanisms derived from animal studies.
Methods: A literature search was performed using PubMed and bibliographies of all relevant original research articles and reviews.
Results: We define 'periconception' as a 5-6-month period in women embracing oocyte growth, fertilization, conceptus formation and development to Week 10 of gestation (coinciding with the closure of the secondary palate in the embryo). During this period significant epigenetic modifications to chromatin occur that correspond with normal development. Subtle variations in 1-C metabolism genes and deficiencies in 1-C substrates/cofactors together with poor lifestyle, such as smoking and alcohol consumption, disturb 1-C metabolism and contribute to subfertility and early miscarriage and compromise offspring health. Procedures used in assisted reproduction can also disturb these metabolic pathways and contribute to poor pregnancy outcomes.
Conclusions: Evidence presented indicates that parental nutrition and other lifestyle factors during the periconceptional period can affect reproductive performance via 1-C metabolic pathways. This knowledge provides opportunities for treatment and prevention of reproductive failures and future non-communicable diseases.
https://www.ncbi.nlm.nih.gov/pubmed/23959022
Association between serum folate and vitamin B-12 and outcomes of assisted reproductive technologies.
Gaskins AJ1, Chiu YH2, Williams PL3, Ford JB4, Toth TL5, Hauser R6, Chavarro JE7; EARTH Study Team
Abstract:
Background: Preconceptional folate and vitamin B-12 have been linked to beneficial reproductive outcomes in both natural pregnancies and those after assisted reproductive technology (ART) treatment.
Objective: The objective of the study was to evaluate the associations of serum folate and vitamin B-12 with ART outcomes.
Design: This analysis included a random sample of 100 women (154 ART cycles) participating in a prospective cohort study [Environment and Reproductive Health (EARTH)] at the Massachusetts General Hospital Fertility Center (2007-2013). Serum folate and vitamin B-12 were measured in blood samples collected between days 3 and 9 of treatment. Generalized estimating equations with adjustment for age, BMI, and race were used to evaluate the association of serum folate and vitamin B-12 with ART outcomes.
Results: Women in the highest quartile of serum folate (>26.3 ng/mL) had 1.62 (95% CI: 0.99, 2.65) times the probability of live birth compared with women in the lowest quartile (<16.6 ng/mL). Women in the highest quartile of serum vitamin B-12 (>701 pg/mL) had 2.04 (95% CI: 1.14, 3.62) times the probability of live birth compared with women in the lowest quartile (<439 pg/mL). Suggestive evidence of an interaction was observed; women with serum folate and vitamin B-12 concentrations greater than the median had 1.92 (95% CI: 1.12, 3.29) times the probability of live birth compared with women with folate and vitamin B-12 concentrations less than or equal to the median. This translated into an adjusted difference in live birth rates of 26% (95% CI: 10%, 48%; P = 0.02).
Conclusion: Higher serum concentrations of folate and vitamin B-12 before ART treatment were associated with higher live birth rates among a population exposed to folic acid fortification. This trial was registered at clinicaltrials.gov as NCT00011713.
Fertilichron male Research:
Improvement in human semen quality after oral supplementation of vitamin C (n=13, open trail per 2 month).
Akmal Met al., J Med Food 2006
Abstract: This study was carried out to monitor the effect of oral supplementation of vitamin C on various semen parameters in oligospermic, infertile, otherwise healthy individuals. Various semen parameters, including sperm motility, sperm count, and sperm morphology, were studied before and after the vitamin C treatment. A total of 13 infertile patients were included. Their ages ranged between 25 and 35 years. They had no genital infection or varicocele. Physical examination and other routine laboratory investigations were normal. General semen analysis revealed oligozoospermia (mean sperm count was 14.3 +/- 7.38 x 10(6) sperms/mL, mean sperm with normal morphology was 43 +/- 7.87%, and mean sperm motility was 31.2 +/- 9.61%). Testicular biopsy was not done. These patients received in an open trial of 1,000 mg of vitamin C twice daily for a maximum of 2 months. Results showed that the mean sperm count was increased to 32.8 +/- 10.3 x 10(6) sperms/mL (P < .001) after 2 months of vitamin C intake. The mean sperm motility was increased significantly to 60.1 +/- 8.47% (P < .001), and mean sperms with normal morphology increased significantly to 66.7 +/- 4.77% (P < .001). This study showed that vitamin C supplementation in infertile men might improve sperm count, sperm motility, and sperm morphology and might have a place as an additional supplement to improve the semen quality towards conception.
Sperm quality improvement after natural anti-oxidant treatment of asthenoteratospermic men with leukocytospermia.
(n=51, controlled trail per 3 month).
Piomboni Pet al., Asian J Androl 2008
Abstract Aim: To study the immune-modulating and anti-oxidant effects of beta-glucan, papaya, lactoferrin, and vitamins C and E on sperm characteristics of patients with asthenoteratozoospermia associated with leucocytosis.
Methods: Fifty-one patients referred to our Sterility Center for semen analysis were selected. Sperm parameters were assessed before and after patient’s treatment with beta-glucan, lactoferrin, papaya, and vitamins C and E. DNA damage was assessed by the acridine orange test and sperm structural characteristics were evaluated by transmission electron microscopy.
Results: After 90 days of treatment, an increase in the percentage of morphologically normal sperm (17.0 ± 5.2 vs. 29.8 ± 6.5) and total progressive motility (19.0 ± 7.8 vs. 34.8 ± 6.8) were detected. Structural sperm characteristics as well as chromatin integrity were also improved after treatment. In terms of leukocyte concentration in seminal fluid, a significant reduction was recorded (2.2 ± 0.9 vs. 0.9 ± 0.2).
Conclusion: The treatment of an inflammatory process by the synergic action of immune modulators and anti-oxidants could protect sperm during maturation and migration, leading to improved sperm function. (Asian J Androl 2008 ***; 10: – )
http://www.progine.it/Sperm%20quality.pdf
Indications of the mechanisms involved in improved sperm parameters by zinc therapy(n=45, controlled trail per 3 month).
Omu AEet al., Med Princ Pract 2008
Abstract:
Objective:To determine possible indications of the mechanisms involved in improved sperm parameters by zinc therapy in asthenozoospermic men.
Subjects and Methods: Forty-five men with asthenozoospermia (>or=40% immotile sperm) were randomized into four therapy groups: zinc only: n = 11; zinc + vitamin E: n = 12 and zinc + vitamins E + C: n = 14 for 3 months, and non-therapy control group: n = 8. Semen analysis was done according to WHO guidelines. Malone dialdehyde, tumour necrosis factor-alpha (TNF-alpha), total antioxidant capacity, superoxide dismutase (SOD) and glutathione peroxidase were determined in the semen and serum. Antisperm antibodies IgG, IgM and IgA were evaluated by immunobeads. Sperm chromatin integrity was determined by acid denaturation by acridine orange and sperm apoptosis by light and electron microscopy. The effect of zinc on in vitro induced sperm oxidative stress by NADH was evaluated.
Results: Asthenozoospermia was significantly associated with oxidative stress with higher seminal malone dialdehyde (8.8 vs. 1.8 mmol/l, p < 0.001) and TNF-alpha (60 vs. 12 pg/l, p < 0.001), and low total antioxidant capacity (1.8 vs. 8.4, p < 0.01), SOD (0.8 vs. 3.1, p < 0.01) and glutathione peroxidase (1.6 vs. 4.2, p < 0.05), compared to normozoospermia. Zinc therapy alone, in combination with vitamin E or with vitamin E + C were associated with comparably improved sperm parameters with less oxidative stress, sperm apoptosis and sperm DNA fragmentation index (DFI). On the whole, there was no difference in the outcome measures between zinc only and zinc with vitamin E and combination of vitamins E + C. In the in vitro experiment zinc supplementation resulted in significantly lower DFI (14-29%, p < 0.05) compared to zinc deficiency.
Conclusion: Zinc therapy reduces asthenozoospermia through several mechanisms such as prevention of oxidative stress, apoptosis and sperm DNA fragmentation.
Male Infertility: The Effect of Natural Antioxidants and Phytocompounds on Seminal Oxidative Stress
Article (PDF Available) · March 2017 with 184 Reads
DOI: 10.3390/diseases5010009
Abstract:Defective sperm function has been identified as the most common cause of infertility. The objective of this study was to review recent findings on the effects of various antioxidants on male fertility. High amounts of poly unsaturated fatty acid are found in the mammalian spermatozoa membranes, thereby making them susceptible to lipid peroxidation. Although, free radicals and reactive oxygen species (ROS) play major roles in reproduction, they are strongly associated with oxidative stress. Furthermore, factors such as obesity, inflammation, pollutants and cigarette smoking are negatively correlated with spermatogenesis. Endogenous antioxidants system exists to mediate these damages. In a normal physiological state, the seminal plasma contains antioxidant enzyme mechanism that is capable of quenching these ROS as well as protecting the spermatozoa against any likely damage. However, high level of ROS triggered by inflammatory cells and oxidation of fatty acid in obese subjects may down play antioxidant mechanism resulting in oxidative stress. Evaluation of such oxidative stress is the first step in the treatment of male infertility through administration of suitable antioxidant. Notably, antioxidant such as vitamin E and C, carotenoids and carnitine have been found beneficial in restoring a balance between ROS generation and scavenging activities. There are emerging evidences that herbal products can also boost male reproductive functions. Nonetheless, a good lifestyle, regular exercise, avoidance of stress and observing safety rules at work are habits that can reverse male infertility.
Discover the world's research
(PDF) Male Infertility: The Effect of Natural Antioxidants and Phytocompounds on Seminal Oxidative Stress. Available from: https://www.researchgate.net/publication/314202739_Male_Infertility_The_Effect_of_Natural_Antioxidants_and_Phytocompounds_on_Seminal_Oxidative_Stress
Fertilichron female Research:
Antioxidant capacity of follicular fluid from patients undergoing in vitro fertilization.
Huang B1, Li Z1, Ai J1, Zhu L1, Li Y1, Jin L1, Zhang H1.
Abstract: This study measured the antioxidant activity of follicular fluid (FF) in infertile patients and assessed its possible correlation between ovarian stimulation and pregnancy outcomes. Samples from 191 infertile patients undergoing in vitro fertilization-embryo transfer (IVF-ET) were determined by α-diphenyl-β-picrylhydrazyl (DPPH) radical scavenging, reducing power, superoxide radical scavenging, β-Carotene bleaching assay, ferrothiocyanate and thiobarbituric acid assays. The comparison between a positive IVF outcome and FF's antioxidant activity was also studied. The results showed FF had strong antioxidant activity, which equated to common antioxidants Vc and BHT (100 μg/mL). Patients with endometriosis had less efficient antioxidant activity in FF than that of patients with tubal occlusion or polycystic ovary syndrome. In conclusion, this study detected, for the first time, the antioxidant activity of FF from patients undergoing an IVF and the FF exhibited strong antioxidant activity.
Keywords: Antioxidant activity; endometriosis; follicular fluid; in vitro fertilization
https://www.ncbi.nlm.nih.gov/pubmed/24966936
Micronutrition and fertility problems in women: What is essential?
Article · April 2017 with 3 Reads
Abstract: New way of life of modern women (tobacco, alcohol, polluted environment, industrial food, endocrine disruptor, etc.) causes an increase of production of reactive oxygen species that affect female fertility. It was found that oxidative stress may damage the oocytes and may impair their fertilization capacity. The aim of this review of recent studies is to select natural ingredients able to reduce oxidative stress. A combination of vitamins (B, C and E), minerals (selenium, iodine) and myo-inositol could be useful as an alternative way, on top of balanced diet and lifestyle advice, for women planning to become pregnant including those with or without SOPK.
Micronutrition and fertility problems in women: What is essential?. Available from: https://www.researchgate.net/publication/319078771_Micronutrition_and_fertility_problems_in_women_What_is_essential?ev=publicSearchHeader&_sg=OLkflgbUBKR-DW8BnuhjARU6gATKsqVmAZziZwYqFsGhEAPbuv8Sktg1NM4DT_khpyLjwXNZ0JcnnAw[accessed Aug 30 2018].
The effect of micronutrient supplements on female fertility.
Abstract:
Purpose of Review: Benefit of micronutrient supplementation on female fertility.
Recent Findings: Reports of randomized trials are rare. Most studies are focused on multivitamin supplementations. For some micronutrients, a positive impact on fertility could be shown. This article reviews the available clinical studies as well as the pathophysiological background of possible effects and summarizes the potential benefits of selected micronutrients on female fertility.
Summary: Apart from lowering the malformation risk by periconceptional supplementation of folic acid, substitution with different micronutrients, particularly folic acid, vitamin B6, vitamin C, vitamin D, vitamin E, iodine, selenium, iron, and DHA might have a positive impact on infertility treatment. The multivitamin formulation should take the pathophysiology, clinical studies, and upper limits into account.
https://www.ncbi.nlm.nih.gov/pubmed/23571830
Antioxidants for female subfertility.
Showell MG1, Mackenzie-Proctor R, Jordan V, Hart RJ.
Abstract:
Background: A couple may be considered to have fertility problems if they have been trying to conceive for over a year with no success. This may affect up to a quarter of all couples planning a child. It is estimated that for 40% to 50% of couples, subfertility may result from factors affecting women. Antioxidants are thought to reduce the oxidative stress brought on by these conditions. Currently, limited evidence suggests that antioxidants improve fertility, and trials have explored this area with varied results. This review assesses the evidence for the effectiveness of different antioxidants in female subfertility.
Objectives: To determine whether supplementary oral antioxidants compared with placebo, no treatment/standard treatment or another antioxidant improve fertility outcomes for subfertile women.
Search Methods: We searched the following databases (from their inception to September 2016) with no language or date restriction: Cochrane Gynaecology and Fertility Group (CGFG) specialised register, the Cochrane Central Register of Studies (CENTRAL CRSO), MEDLINE, Embase, PsycINFO, CINAHL and AMED. We checked reference lists of appropriate studies and searched for ongoing trials in the clinical trials registers.
Selection Criteria: We included randomized controlled trials (rcts) that compared any type, dose or combination of oral antioxidant supplement with placebo, no treatment or treatment with another antioxidant, among women attending a reproductive clinic. We excluded trials comparing antioxidants with fertility drugs alone and trials that only included fertile women attending a fertility clinic because of male partner infertility.
Data Collection and Analysis: Two review authors independently selected eligible studies, extracted the data and assessed the risk of bias of the included studies. The primary review outcome was live birth; secondary outcomes included clinical pregnancy rates and adverse events. We pooled studies using a fixed-effect model, and calculated odds ratios (ors) with 95% confidence intervals (cis) for the dichotomous outcomes of live birth, clinical pregnancy and adverse events. We assessed the overall quality of the evidence by applying grade criteria.
Main Results: We included 50 trials involving 6510 women. Investigators compared oral antioxidants, including combinations of antioxidants, N-acetyl-cysteine, melatonin, L-arginine, myo-inositol, D-chiro-inositol, carnitine, selenium, vitamin E, vitamin B complex, vitamin C, vitamin D+calcium, CoQ10, pentoxifylline and omega-3-polyunsaturated fatty acids versus placebo, no treatment/standard treatment or another antioxidant.Very low-quality evidence suggests that antioxidants may be associated with an increased live birth rate compared with placebo or no treatment/standard treatment (OR 2.13, 95% CI 1.45 to 3.12, P > 0.001, 8 RCTs, 651 women, I2 = 47%). This suggests that among subfertile women with an expected live birth rate of 20%, the rate among women using antioxidants would be between 26% and 43%.Very low-quality evidence suggests that antioxidants may be associated with an increased clinical pregnancy rate compared with placebo or no treatment/standard treatment (OR 1.52, 95% CI 1.31 to 1.76, P < 0.001, 26 RCTs, 4271 women, I2 = 66%). This suggests that among subfertile women with an expected clinical pregnancy rate of 22%, the rate among women using antioxidants would be between 27% and 33%. Heterogeneity was moderately high.There was insufficient evidence to determine whether there was a difference between the groups in rates of miscarriage (OR 0.79, 95% CI 0.58 to 1.08, P = 0.14, 18 RCTs, 2834 women, I2 = 23%, very low quality evidence). This suggests that, among subfertile women with an expected miscarriage rate of 7%, use of antioxidants would be expected to result in a miscarriage rate of between 4% and 7%. There was also insufficient evidence to determine whether there was a difference between the groups in rates of multiple pregnancy (OR 1.00, 95% CI 0.73 to 1.38, P = 0.98, 8 RCTs, 2163 women, I2 = 4%, very low quality evidence). This suggests that among subfertile women with an expected multiple pregnancy rate of 8%, use of antioxidants would be expected to result in a multiple pregnancy rate between 6% and 11%. Likewise, there was insufficient evidence to determine whether there was a difference between the groups in rates of gastrointestinal disturbances (OR 1.55, 95% CI 0.47 to 5.10, P = 0.47, 3 RCTs, 343 women, I2 = 0%, very low quality evidence). This suggests that among subfertile women with an expected gastrointestinal disturbance rate of 2%, use of antioxidants would be expected to result in a rate between 1% and 11%. Overall adverse events were reported by 35 trials in the meta-analysis, but there was insufficient evidence to draw any conclusions. Only one trial reported on live birth, clinical pregnancy or adverse effects in the antioxidant versus antioxidant comparison, and no conclusions could be drawn.Very low-quality evidence suggests that pentoxifylline may be associated with an increased clinical pregnancy rate compared with placebo or no treatment (OR 2.07, 95% CI 1.20 to 3.56, P = 0.009, 3 RCTs, 276 women, I2 = 0%). This suggests that among subfertile women with an expected clinical pregnancy rate of 25%, the rate among women using pentoxifylline would be between 28% and 53%.There was insufficient evidence to determine whether there was a difference between the groups in rates of miscarriage (OR 1.34, 95% CI 0.46 to 3.90, P = 0.58, 3 RCTs, 276 women, I2 = 0%) or multiple pregnancy (OR 0.78, 95% CI 0.20 to 3.09, one RCT, 112 women, very low quality evidence). This suggests that among subfertile women with an expected miscarriage rate of 4%, the rate among women using pentoxifylline would be between 2% and 15%. For multiple pregnancy, the data suggest that among subfertile women with an expected multiple pregnancy rate of 9%, the rate among women using pentoxifylline would be between 2% and 23%.The overall quality of evidence was limited by serious risk of bias associated with poor reporting of methods, imprecision and inconsistency.
Authors' Conclusions: In this review, there was very low-quality evidence to show that taking an antioxidant may provide benefit for subfertile women, but insufficient evidence to draw any conclusions about adverse events. At this time, there is limited evidence in support of supplemental oral antioxidants for subfertile women.
https://www.ncbi.nlm.nih.gov/pubmed/28752910
Female dietary antioxidant intake and time to pregnancy among couples treated for unexplained infertility.
Ruder EH1, Hartman TJ2, Reindollar RH3, Goldman MB4.
Abstract:
Objective: To determine whether increased antioxidant intake in women is associated with shorter time to pregnancy (ttp) among a cohort of couples being treated for unexplained infertility.
Design: Secondary data analysis of a randomized controlled trial.
Setting: Academic medical center associated with a private infertility center.
Patients: Females with unexplained infertility.
Interventions: None.
Main Outcome Measure(s): The time it took to establish a pregnancy that led to a live birth.
Result: Mean nutrient intake exceeded the estimated average requirement (ear) for vitamins c and e. No differences in mean intake of any of the antioxidants were noted between women who delivered a live-born infant during the study period vs. Those who did not. In multivariable models, intake of β-carotene from dietary supplements was associated with shorter ttp among women with body mass index (bmi) ≥25 kg/m(2) (hazard ratio [hr] 1.29, 95% confidence interval [ci] 1.09-1.53) and women <35 y (hr 1.19, 95% ci 1.01-1.41). Intake of vitamin c from dietary supplements was associated with shorter ttp among women with bmi <25 kg/m(2) (hr 1.09, 95% ci 1.03-1.15) and women <35 y (hr 1.10, 95% ci 1.02-1.18). Intake of vitamin e from dietary supplements among women ≥35 y also was associated with shorter ttp (hr 1.07, 95% ci 1.01-1.13).
Conclusions: Shorter TTP was observed among women with BMI <25 kg/m(2) with increasing vitamin C, women with BMI ≥25 kg/m(2) with increasing β-carotene, women <35 y with increasing β-carotene and vitamin C, and women ≥35 y with increasing vitamin E.
CLINICAL TRIAL REGISTRATION NUMBER:
Fertilichron male Research:
The Effects of Combined Oral Antioxidants on Male Infertility
Article in International Journal of Research in Pharmaceutical Sciences9(SPL1) · April 2018 with 6 Reads
DOI: 10.26452/ijrps.v9iSPL1.1290
Abstract: High reactive oxygen species (ROS) levels was considered as an important factor of male infertility that can result in DNA damage, decrease motility and damage membrane integrity. The role of antioxidants is to maintain the balance between ROS production and their clearance which improve sperm parameters and enhance male fertility. Sixty six male patients with median age of 29 years with a mean period of infertility of 1.5 year that attend the infertility clinic in Al-Diwaniya Maternity and Pediatric Hospital were selected randomly in this study which extend from January 2013 to October 2014 (22 months).The patients were selected to have idiopathic oligo-astheno-teratozoospermia,they underwent a detailed history,general and genital physical examination,Two semen analyses,baseline hormone profile and scrotal Doppler ultrasound examination. All patients were given a combination of oral antioxidants including vitamin E (400 IU. once daily), coenzyme Q10 (75 mg. tablet twice a day),zinc sulphate (15 mg. tablet three time a day) and L-carnitine (1000 mg. twice a day) for three months duration of treatment. Semen analysis was repeated after three months from initiation of therapy and was evaluated for changes in volume, concentration, motility and morphology in comparison with baseline semen analyses and any pregnancy was also documented. Thirteen patients (19%) get pregnancy after a period of 2 to 3 months, other patients show variable changes in their seminal analysis after 3 months. Thirty patients (45%) show increasing in seminal volume of 0.5 to 2 ml., while the sperm concentration was increased in 28 patients (42%). Twenty two patients (33%) show increasing in motility, morphology was increased in 34 patients (51%).From all 66 patients; 6 patients (9 %) get improvement in all four parameters, while 9 patients (14 %) get improvement in only 3 parameters,20 patients (30 %) get improvement in only 2 parameters,23 patients (35 %) get improvement in only one parameter and 8 patients (12 %) had no improvement in any parameter. This study demonstrates a possible role of combined oral antioxidants in the improvement of semen parameters and pregnancy rate for selected infertile men with superiority for the use of combination of antioxidants rather than single agent treatment.
The Effects of Combined Oral Antioxidants on Male Infertility. Available from: https://www.researchgate.net/publication/324777229_The_Effects_of_Combined_Oral_Antioxidants_on_Male_Infertility
Does Vitamin D Deficiency Have a Role in the Reduced Fertility?
Article (PDF Available) · January 2018 with 54 Reads
DOI: 10.1016/j.rpedm.2017.10.058
Abstract: Vitamin D is an emerging factor influencing fertility. The basis of this relationship lays on the presence of both vitamin D receptor and 1α-hydroxylase enzyme in reproductive organs. The widespread of vitamin D deficiency across all age groups and the published studies about the negative impact on overall health led to several investigations to assess the effect of vitamin D levels in human reproduction. Vitamin D status correlates to metabolic and hormonal dysfunctions in women with polycystic ovary syndrome and vitamin D deficiency is a negative predictor of ovulatory response in those women. Also, a positive correlation between vitamin D levels and anti-Müllerian hormone have been documented. Evidence suggests a link between lower vitamin D status, and endometriosis and vitamin supplementation has been associated with amelioration of dysmenorrhea. Studies in men revealed a positive correlation between circulating vitamin D levels and semen quality parameters. Vitamin D supplementation is being considered to improve semen quality in at least some of the idiopathic cases of male infertility. The relationship between vitamin D levels and assisted reproductive techniques outcomes have also been investigated, although the results are controversial. This paper intends to review the latest knowledge concerning the role of vitamin D in human reproduction.
(PDF) Does Vitamin D Deficiency Have a Role in the Reduced Fertility?. Available from: https://www.researchgate.net/publication/322764561_Does_Vitamin_D_Deficiency_Have_a_Role_in_the_Reduced_Fertility[accessed Aug 23 2018].
Homeostatic Relevance of Vitamin D in Maintaining Male Fertility in Human: Down-regulation of Oxidative Stress and Upregulation of Anti-oxidative Defence and Steroidal Hormones
Article (PDF Available) · January 2018 with 160 Reads
DOI: 10.4103/2305-0500.228014
Abstract:
Background: Vitamin D deficiency is one of the leading causes of different reproductive defects including hypogonadism, miscarriage, and pre-term births. The role of vitamin D has been well established in human reproduction system by the regulation of sex steroid hormones such as testosterone and specific pituitary secretions including luteinizing hormone (LH) and follicle-stimulating hormone (FSH). The aim of the present research was to evaluate correlation between the levels of vitamin D and male infertility as well as to determine the efficacy of vitamin D in improving the male fertility by up-regulating the levels of testosterone and spermatogenesis.
Methods: In the present study, fifty (50) male patients having fertility defects (ages 25-70 years) were screened and 50 healthy individuals were taken as control. All human subjects were screened for 4-HNE, isoprostane-F2α (IP-F2α), 8-OHdG, vitamin D, luteinizing hormone (LH), follicle stimulating hormone (FSH), testosterones, malondialdehyde (MDA), superoxide dismutase (SOD), catalase (CAT), glutathione peroxidase (GSH), and NO.
Results: The screening analysis revealed that the levels of LH, FSH, and testosterone were lower in male infertile subjects (6.29 ± 0.54 mU/mL), (5.29 ± 0.51 mU/mL), and (14.26 ± 1.31 ng/dL) compared to healthy subjects (11.19 ± 1.25 mU/mL), (9.57 ± 0.83 mU/mL), and (25.29 ± 2.53 ng/dL), respectively. Similarly, the levels of vitamin D (17.17 ± 2.30 ng/mL) and calcium (6.29 ± 0.31 mg/dL) were significantly lesser in infertile groups compared to the normal healthy groups. Moreover, we observed that the levels of SOD, CAT, and GSH were significantly higher in healthy subjects compared to the infertile subjects.
Conclusion: Vitamin D exhibits strong relevance to male fertility by maintaining the levels of sex hormones (LH, FSH, and testosterone), up-regulating the antioxidant defense (SOD, CAT, and GSH), and down-regulating the oxidative stress (MDA, NO, and iNOS species).
(PDF) Homeostatic Relevance of Vitamin D in Maintaining Male Fertility in Human: Down-regulation of Oxidative Stress and Upregulation of Anti-oxidative Defence and Steroidal Hormones. Available from: https://www.researchgate.net/publication/322487095_Homeostatic_Relevance_of_Vitamin_D_in_Maintaining_Male_Fertility_in_Human_Down-regulation_of_Oxidative_Stress_and_Upregulation_of_Anti-oxidative_Defence_and_Steroidal_Hormones
The role of vitamin D in male fertility: A focus on the testis
Article (PDF Available) in Reviews in Endocrine and Metabolic Disorders18(Suppl 1) · July 2017 with 206 Reads
DOI: 10.1007/s11154-017-9425-0
Abstract: In the last decade, vitamin D has emerged as a pleiotropic molecule with a multitude of autocrine, paracrine and endocrine functions, mediated by classical genomic as well as non-classical non-genomic actions, on multiple target organs and systems. The expression of vitamin D receptor and vitamin D metabolizing enzymes in male reproductive system, particularly in the testis, suggests the occurrence of vitamin D synthesis and regulation as well as function in the testis. The role of vitamin D in the modulation of testis functions, including hormone production and spermatogenesis, has been investigated in animals and humans. Experimental studies support a beneficial effect of vitamin D on male fertility, by modulating hormone production through genomic and non-genomic actions, and, particularly, by improving semen quality essentially through non-genomic actions. However, clinical studies in humans are controversial. Indeed, vitamin D seems to contribute to the modulation of the bioavailable rather than total testosterone. Moreover, although an increased prevalence or risk for testosterone deficiency was reported in men with vitamin D deficiency in observational studies, the majority of interventional studies demonstrated the lack of effect of vitamin D supplementation on circulating levels of testosterone. The most consistent effect of vitamin D was reported on semen quality. Indeed, vitamin D was shown to be positively associated to sperm motility, and to exert direct actions on spermatozoa, including non-genomic driven modulation of intracellular calcium homeostasis and activation of molecular pathways involved in sperm motility, capacitation and acrosome reaction. The current review provides a summary of current knowledge on the role of vitamin D in male fertility, by reporting clinical and experimental studies in humans and animals addressing the relationship between vitamin D and testis function.
(PDF) The role of vitamin D in male fertility: A focus on the testis. Available from: https://www.researchgate.net/publication/318099900_The_role_of_vitamin_D_in_male_fertility_A_focus_on_the_testis
Fertilichron female Research:
Effect of vitamin D status on clinical pregnancy rates following in vitro fertilization.
Garbedian K1, Boggild M2, Moody J3, Liu KE1.
Abstract:
Background: Recent studies suggest that vitamin d may play a role in human reproduction. Our goal was to investigate whether vitamin d levels are predictive of implantation and clinical pregnancy rates in infertile women following in vitro fertilization (ivf).
Methods: We prospectively evaluated vitamin d status, as determined by serum 25-hydroxy-vitamin d (25[oh]d) levels, in a cohort of 173 women undergoing ivf at mount sinai hospital, toronto, ontario. Serum 25(oh)d samples were collected within 1 week before oocyte retrieval. We classified patients as having sufficient (≥ 75 nmol/l) or insufficient (or deficient; hereafter referred to as "insufficient"; < 75 nmol/l) serum levels of 25(oh)d. We compared patient demographics and ivf cycle parameters between groups. The primary outcome measure was clinical pregnancy (intrauterine sac visible on ultrasound performed 4-5 weeks after embryo transfer).
Results: Of the included women, 54.9% had insufficient 25(OH)D levels and 45.1% had sufficient levels. Women with sufficient levels had significantly higher rates of clinical pregnancy per IVF cycle started (52.5%) compared with women with insufficient levels (34.7%; p < 0.001). Implantation rates were also higher in the sufficient 25(OH)D group, but the results were not statistically significant. Multivariable logistic regression analysis (adjusted for age, body mass index and day 5 [v. day 3] embryo transfer) showed that serum 25(OH)D level may be a predictor of clinical pregnancy (adjusted odds ratio 1.01, 95% confidence interval 1.00-1.03).
Interpretation: Our findings suggest that women with sufficient levels of vitamin d are significantly more likely to achieve clinical pregnancy following ivf. Vitamin d supplementation could provide an easy and cost-effective way of improving pregnancy rates; this merits further investigation.
Trial Registration:
ClinicalTrials.gov, no. NCT01348594.
https://www.ncbi.nlm.nih.gov/pubmed/25077107
Replete vitamin D stores predict reproductive success following in vitro fertilization.
Ozkan S1, Jindal S, Greenseid K, Shu J, Zeitlian G, Hickmon C, Pal L.
Abstract:
Objective: To determine whether 25oh-d levels in the follicular fluid (ff) of infertile women undergoing IVF demonstrate a relationship with IVF cycle parameters and outcome, hypothesizing that levels of 25oh-d in body fluids are reflective of vitamin repletion status.
Design: Prospective cohort study.
Setting: Academic tertiary care center.
Patient(s): Eighty-four infertile women undergoing IVF.
Intervention(s): Follicular fluid from follicles>or=14 mm; serum (n = 10) and ff levels of 25oh-d.
Main Outcome Measure(s): Clinical pregnancy (CP), defined as evidence of intrauterine gestation sac on ultrasound, following IVF; IVF cycle parameters.
Result(s): Serum and ff levels of 25oh-d were highly correlated (r=0.94). In a predominantly caucasian population (66%), significantly lower ff 25oh-d levels were noted in black versus non-black patients. Significant inverse correlations were seen between ff 25oh-d levels and body mass index (r=-0.25). Significantly higher cp and implantation rates were observed across tertiles of ff25oh-d; patients achieving cp following ivf (n=26) exhibited significantly higher ff levels of 25oh-d. Multivariable logistic regression analysis confirmed ff 25oh-d levels as an independent predictor to success of an ivf cycle; adjusting for age, body mass index, ethnicity, and number of embryos transferred, each ng/ml increase in ff 25oh-d increased the likelihood for achieving cp by 6%.
Conclusion(s): Our findings that women with higher vitamin D level in their serum and FF are significantly more likely to achieve CP following IVF-embryo transfer are novel. A potential for benefit of vitamin D supplementation on treatment success in infertile patients undergoing IVF is suggested and merits further investigation.
https://www.ncbi.nlm.nih.gov/pubmed/19589516
Vitamin D and women’s reproductive health (literature review)
Article · July 2018 with 2 Reads
DOI: 10.21518/2079-701X-2018-12-164-172
Abstract: Vitamin D and women’s reproductive health (literature review). Literature search the relationship between vitamin D and fertility in women performed in Pubmed. The vitamin D receptor (VDR) and vitamin D metabolizing enzymes are found in reproductive tissues of women. Moreover, we present evidence that vitamin D is involved in female reproduction including IVF outcome and polycystic ovary syndrome (PCOS). In PCOS women, low 25-hydroxyvitamin D (25(OH)D) levels are associated with obesity, metabolic, and endocrine disturbances and vitamin D supplementation might improve menstrual frequency and metabolic disturbances in those women. Moreover, vitamin D might influence steroidogenesis of sex hormones (estradiol and progesterone) in healthy women and high 25(OH)D levels might be associated with endometriosis.
Vitamin D and women’s reproductive health (literature review). Available from: https://www.researchgate.net/publication/326686623_Vitamin_D_and_women%27s_reproductive_health_literature_review?ev=publicSearchHeader&_sg=wM3rNekAX1YmaeLikO5Bfa6x57TPTvEkLVnU5l4MyCbBXE-arQCtytdtl19cAVfoey2z1dMDpwD86_s
The effect of micronutrient supplements on female fertility.
Abstract:
Purpose of Review: Benefit of micronutrient supplementation on female fertility.
Recent Findings: Reports of randomized trials are rare. Most studies are focused on multivitamin supplementations. For some micronutrients, a positive impact on fertility could be shown. This article reviews the available clinical studies as well as the pathophysiological background of possible effects and summarizes the potential benefits of selected micronutrients on female fertility.
Summary: Apart from lowering the malformation risk by periconceptional supplementation of folic acid, substitution with different micronutrients, particularly folic acid, vitamin B6, vitamin C, vitamin D, vitamin E, iodine, selenium, iron, and DHA might have a positive impact on infertility treatment. The multivitamin formulation should take the pathophysiology, clinical studies, and upper limits into account.
https://www.ncbi.nlm.nih.gov/pubmed/23571830
Antioxidants for female subfertility.
Showell MG1, Mackenzie-Proctor R, Jordan V, Hart RJ.
Abstract:
Background: A couple may be considered to have fertility problems if they have been trying to conceive for over a year with no success. This may affect up to a quarter of all couples planning a child. It is estimated that for 40% to 50% of couples, subfertility may result from factors affecting women. Antioxidants are thought to reduce the oxidative stress brought on by these conditions. Currently, limited evidence suggests that antioxidants improve fertility, and trials have explored this area with varied results. This review assesses the evidence for the effectiveness of different antioxidants in female subfertility.
Objectives: To determine whether supplementary oral antioxidants compared with placebo, no treatment/standard treatment or another antioxidant improve fertility outcomes for subfertile women.
Search Methods: We searched the following databases (from their inception to September 2016) with no language or date restriction: Cochrane Gynecology and Fertility Group (CGFG) specialized register, the Cochrane Central Register of Studies (CENTRAL CRSO), MEDLINE, Embase, PsycINFO, CINAHL and AMED. We checked reference lists of appropriate studies and searched for ongoing trials in the clinical trials registers.
Selection Criteria: We included randomized controlled trials (RCTs) that compared any type, dose or combination of oral antioxidant supplement with placebo, no treatment or treatment with another antioxidant, among women attending a reproductive clinic. We excluded trials comparing antioxidants with fertility drugs alone and trials that only included fertile women attending a fertility clinic because of male partner infertility.
Data Collection and Analysis: Two review authors independently selected eligible studies, extracted the data and assessed the risk of bias of the included studies. The primary review outcome was live birth; secondary outcomes included clinical pregnancy rates and adverse events. We pooled studies using a fixed-effect model, and calculated odds ratios (ORs) with 95% confidence intervals (CIs) for the dichotomous outcomes of live birth, clinical pregnancy and adverse events. We assessed the overall quality of the evidence by applying GRADE criteria.
Main Results: We included 50 trials involving 6510 women. Investigators compared oral antioxidants, including combinations of antioxidants, N-acetyl-cysteine, melatonin, L-arginine, myo-inositol, D-chiro-inositol, carnitine, selenium, vitamin E, vitamin B complex, vitamin C, vitamin D+calcium, CoQ10, pentoxifylline and omega-3-polyunsaturated fatty acids versus placebo, no treatment/standard treatment or another antioxidant. Very low-quality evidence suggests that antioxidants may be associated with an increased live birth rate compared with placebo or no treatment/standard treatment (OR 2.13, 95% CI 1.45 to 3.12, P > 0.001, 8 RCTs, 651 women, I2 = 47%). This suggests that among subfertile women with an expected live birth rate of 20%, the rate among women using antioxidants would be between 26% and 43%.Very low-quality evidence suggests that antioxidants may be associated with an increased clinical pregnancy rate compared with placebo or no treatment/standard treatment (OR 1.52, 95% CI 1.31 to 1.76, P < 0.001, 26 RCTs, 4271 women, I2 = 66%). This suggests that among subfertile women with an expected clinical pregnancy rate of 22%, the rate among women using antioxidants would be between 27% and 33%. Heterogeneity was moderately high. There was insufficient evidence to determine whether there was a difference between the groups in rates of miscarriage (OR 0.79, 95% CI 0.58 to 1.08, P = 0.14, 18 RCTs, 2834 women, I2 = 23%, very low quality evidence). This suggests that, among subfertile women with an expected miscarriage rate of 7%, use of antioxidants would be expected to result in a miscarriage rate of between 4% and 7%. There was also insufficient evidence to determine whether there was a difference between the groups in rates of multiple pregnancy (OR 1.00, 95% CI 0.73 to 1.38, P = 0.98, 8 RCTs, 2163 women, I2 = 4%, very low quality evidence). This suggests that among subfertile women with an expected multiple pregnancy rate of 8%, use of antioxidants would be expected to result in a multiple pregnancy rate between 6% and 11%. Likewise, there was insufficient evidence to determine whether there was a difference between the groups in rates of gastrointestinal disturbances (OR 1.55, 95% CI 0.47 to 5.10, P = 0.47, 3 RCTs, 343 women, I2 = 0%, very low quality evidence). This suggests that among subfertile women with an expected gastrointestinal disturbance rate of 2%, use of antioxidants would be expected to result in a rate between 1% and 11%. Overall adverse events were reported by 35 trials in the meta-analysis, but there was insufficient evidence to draw any conclusions. Only one trial reported on live birth, clinical pregnancy or adverse effects in the antioxidant versus antioxidant comparison, and no conclusions could be drawn. Very low-quality evidence suggests that pentoxifylline may be associated with an increased clinical pregnancy rate compared with placebo or no treatment (OR 2.07, 95% CI 1.20 to 3.56, P = 0.009, 3 RCTs, 276 women, I2 = 0%). This suggests that among subfertile women with an expected clinical pregnancy rate of 25%, the rate among women using pentoxifylline would be between 28% and 53%.There was insufficient evidence to determine whether there was a difference between the groups in rates of miscarriage (OR 1.34, 95% CI 0.46 to 3.90, P = 0.58, 3 RCTs, 276 women, I2 = 0%) or multiple pregnancy (OR 0.78, 95% CI 0.20 to 3.09, one RCT, 112 women, very low quality evidence). This suggests that among subfertile women with an expected miscarriage rate of 4%, the rate among women using pentoxifylline would be between 2% and 15%. For multiple pregnancy, the data suggest that among subfertile women with an expected multiple pregnancy rate of 9%, the rate among women using pentoxifylline would be between 2% and 23%.The overall quality of evidence was limited by serious risk of bias associated with poor reporting of methods, imprecision and inconsistency.
Authors' Conclusions: In this review, there was very low-quality evidence to show that taking an antioxidant may provide benefit for subfertile women, but insufficient evidence to draw any conclusions about adverse events. At this time, there is limited evidence in support of supplemental oral antioxidants for subfertile women.
Fertilichron male Research:
Sperm quality improvement after natural anti-oxidant treatment of asthenoteratospermic men with leukocytospermia.
(n=51, controlled trail per 3 month).
Piomboni Pet al., Asian J Androl 2008
Abstract Aim: To study the immune-modulating and anti-oxidant effects of beta-glucan, papaya, lactoferrin, and vitamins C and E on sperm characteristics of patients with asthenoteratozoospermia associated with leucocytosis.
Methods: Fifty-one patients referred to our Sterility Center for semen analysis were selected. Sperm parameters were assessed before and after patient’s treatment with beta-glucan, lactoferrin, papaya, and vitamins C and E. DNA damage was assessed by the acridine orange test and sperm structural characteristics were evaluated by transmission electron microscopy.
Results: After 90 days of treatment, an increase in the percentage of morphologically normal sperm (17.0 ± 5.2 vs. 29.8 ± 6.5) and total progressive motility (19.0 ± 7.8 vs. 34.8 ± 6.8) were detected. Structural sperm characteristics as well as chromatin integrity were also improved after treatment. In terms of leukocyte concentration in seminal fluid, a significant reduction was recorded (2.2 ± 0.9 vs. 0.9 ± 0.2).
Conclusion: The treatment of an inflammatory process by the synergic action of immune modulators and anti-oxidants could protect sperm during maturation and migration, leading to improved sperm function. (Asian J Androl 2008 ***; 10: – ) http://www.progine.it/Sperm%20quality.pdf
Indications of the mechanisms involved in improved sperm parameters by zinc therapy(n=45, controlled trail per 3 month).
Omu AEet al., Med Princ Pract 2008
Abstract:
Objects:To determine possible indications of the mechanisms involved in improved sperm parameters by zinc therapy in asthenozoospermic men.
Subjects and Methods: Forty-five men with asthenozoospermia (>or=40% immotile sperm) were randomized into four therapy groups: zinc only: n = 11; zinc + vitamin E: n = 12 and zinc + vitamins E + C: n = 14 for 3 months, and non-therapy control group: n = 8. Semen analysis was done according to WHO guidelines. Malone dialdehyde, tumour necrosis factor-alpha (TNF-alpha), total antioxidant capacity, superoxide dismutase (SOD) and glutathione peroxidase were determined in the semen and serum. Antisperm antibodies IgG, IgM and IgA were evaluated by immunobeads. Sperm chromatin integrity was determined by acid denaturation by acridine orange and sperm apoptosis by light and electron microscopy. The effect of zinc on in vitro induced sperm oxidative stress by NADH was evaluated.
Results: Asthenozoospermia was significantly associated with oxidative stress with higher seminal malone dialdehyde (8.8 vs. 1.8 mmol/l, p < 0.001) and TNF-alpha (60 vs. 12 pg/l, p < 0.001), and low total antioxidant capacity (1.8 vs. 8.4, p < 0.01), SOD (0.8 vs. 3.1, p < 0.01) and glutathione peroxidase (1.6 vs. 4.2, p < 0.05), compared to normozoospermia. Zinc therapy alone, in combination with vitamin E or with vitamin E + C were associated with comparably improved sperm parameters with less oxidative stress, sperm apoptosis and sperm DNA fragmentation index (DFI). On the whole, there was no difference in the outcome measures between zinc only and zinc with vitamin E and combination of vitamins E + C. In the in vitro experiment zinc supplementation resulted in significantly lower DFI (14-29%, p < 0.05) compared to zinc deficiency.
Conclusion: Zinc therapy reduces asthenozoospermia through several mechanisms such as prevention of oxidative stress, apoptosis and sperm DNA fragmentation.
Antioxidants and Phytocompounds on Seminal Oxidative Stress
Article (PDF Available) · March 2017 with 184 Reads
DOI: 10.3390/diseases5010009
Abstract: Defective sperm function has been identified as the most common cause of infertility. The objective of this study was to review recent findings on the effects of various antioxidants on male fertility. High amounts of poly unsaturated fatty acid are found in the mammalian spermatozoa membranes, thereby making them susceptible to lipid peroxidation. Although, free radicals and reactive oxygen species (ROS) play major roles in reproduction, they are strongly associated with oxidative stress. Furthermore, factors such as obesity, inflammation, pollutants and cigarette smoking are negatively correlated with spermatogenesis. Endogenous antioxidants system exists to mediate these damages. In a normal physiological state, the seminal plasma contains antioxidant enzyme mechanism that is capable of quenching these ROS as well as protecting the spermatozoa against any likely damage. However, high level of ROS triggered by inflammatory cells and oxidation of fatty acid in obese subjects may down play antioxidant mechanism resulting in oxidative stress. Evaluation of such oxidative stress is the first step in the treatment of male infertility through administration of suitable antioxidant. Notably, antioxidant such as vitamin E and C, carotenoids and carnitine have been found beneficial in restoring a balance between ROS generation and scavenging activities. There are emerging evidences that herbal products can also boost male reproductive functions. Nonetheless, a good lifestyle, regular exercise, avoidance of stress and observing safety rules at work are habits that can reverse male infertility.
(PDF) Male Infertility: The Effect of Natural Antioxidants and Phytocompounds on Seminal Oxidative Stress. Available from: https://www.researchgate.net/publication/314202739_Male_Infertility_The_Effect_of_Natural_Antioxidants_and_Phytocompounds_on_Seminal_Oxidative_Stress
One-carbon cycle support rescues sperm damage in experimentally induced varicocoele in rats.
Mohammadi P1,2, Hassani-Bafrani H2,3, Tavalaee M1, Dattilo M4, Nasr-Esfahani MH1,5.
Abstract
Objectives: To investigate whether micronutrients in support of the one-carbon cycle and glutathione synthesis are effective in improving sperm damage after surgical varicocoele induction in rats and whether any effect is achieved without a rebound reductive stress as seen with oral antioxidants.
Materials and Methods: Surgical varicocele was induced in adult male Wistar rats and resulted in significant damage to the testis and sperm cells measured at 2 and 4 months after surgery. At 2 months after surgery, rats received a 2-month oral supplementation in support of the one-carbon cycle containing B vitamins (B2, B3, B6, folic acid and B12), N-acetyl-cysteine, zinc, small amounts of vitamin E, and a natural source of betalains and quercetine (Condensyl® ; Parthenogen SAGL, Lugano, Switzerland and Nurilia SARL, Lyon, France).
Results: One-carbon cycle supplementation, compared to untreated controls, significantly improved the morphometric characteristics of testis (P < 0.05), sperm concentration, motility and abnormal morphology (P < 0.001), sperm chromatin condensation (aniline blue staining, P < 0.05), sperm DNA damage (acridine orange staining, P < 0.05) and sperm lipid peroxidation (BODIPY C11, P < 0.001). The improvement in both nuclear condensation and DNA damage and the lack of excessive inhibition of lipid peroxidation confirmed that no reductive stress had occurred.
Conclusions: Micronutrients in support of the one-carbon cycle are effective in the treatment of surgically induced varicocele in rats, probably by activating natural antioxidant defenses and epigenetics. These results support the idea that essential micronutrients including B vitamins may also have a positive influence in clinical varicocele, which should be tested in prospective clinical trials.
https://www.ncbi.nlm.nih.gov/pubmed/29752770
Lipovac M, Bodner F, Imhof M, Chedraui P.
Reprod Biol Endocrinol.2016 Dec 9;14(1):84.
Comparison of the effect of a combination of eight micronutrients versus a standard mono preparation on sperm parameters.
Abstract
Background: There are reports showing that l-carnitine alone or in combination with other micronutrients improve sperm parameters. However, comparative studies are still lacking. This study was carried out to compare the short term effects of a combination of eight micronutrients including l-carnitine vs. a mono-substance (l-carnitine alone) on sperm parameters.
Methods: This was a prospective, open-labelled, nonrandomized study that included male subjects (20 to 60 years) with at least 1 year of subfertility and at least one pathological semen analysis who received 3 months treatment with a mono-substance (500 mg l-carnitine/twice a day, n = 156) or a combined compound (440 mg l-carnitine + 250 mg l-arginine + 40 mg zinc + 120 mg vitamin E + 80 mg glutathione + 60 μg selenium + 15 mg coenzyme Q10 + 800 μg folic acid/once a day, n = 143) for the same time period. Sperm parameters were analyzed before and after treatment and groups comparisons performed.
Results: Baseline characteristics were similar among studied groups (age and body mass indices). Semen parameters (volume, density, overall progressive motility [including slow and fast motility]) and percentage of sperm with normal morphology improved after 3 months in both groups as compared to baseline. However, relative change (expressed as % increase of absolute values) for sperm density and overall progressive motility (including fast motility) was found to be higher for the combined micronutrient treatment group as compared to the mono-treatment using l-carnitine alone.
Conclusion: Both analyzed groups displayed a positive short-term effect on all sperm parameters; however effect on density and motility was significantly better for the combined formulation. There is need for more research in this matter that includes long term outcome data.
Fertilichron female Research:
Vitamin E effect on controlled ovarian stimulation of unexplained infertile women.
Cicek N1, Eryilmaz OG, Sarikaya E, Gulerman C, Genc Y.
Abstract:
Purpose: To determine Vit E effect on the treatment outcomes of women with unexplained infertility undergoing controlled ovarian stimulation and intrauterine insemination (IUI).
Methods: The study group (Group A, n053) underwent controlled ovarian stimulation with clomiphene citrate with Vit E administration, 400 IU/day p.o. while the control group(Group B, n050) underwent ovulation induction without VitE. Treatment outcomes were compared between the groups.
Results: There were no significant differences between the two groups with respect to the demographic outcomes. The difference in endometrial thickness on the day of hCG administration was significant between the two groups (p00.001). The effect of receiving Vit E on the implantation and the on going pregnancy rates were assessed Odds Ratio (OR) and corresponding 95% Confidence Intervals (CI). Receiving Vit E was not significantly associated with the implantation and the ongoing pregnancy rates; OR 0 1.22, 95% CI (0.44–3.4) and OR 0 1.43, 95% CI (0.49–4.1), respectively.
Conclusion: Vit E administration may improve the endometrial response in unexplained infertile women via the likely antioxidant and the anticoagulant effects. It may also modulate the antiestrogenic effect of clomiphene citrate and the problem of a thin endometrium in these cycles may beadjusted
https://www.ncbi.nlm.nih.gov/pubmed/22302530
Micronutrition and fertility problems in women: What is essential?
Article · April 2017 with 3 Reads
Abstract: New way of life of modern women (tobacco, alcohol, polluted environment, industrial food, endocrine disruptor, etc.) causes an increase of production of reactive oxygen species that affect female fertility. It was found that oxidative stress may damage the oocytes and may impair their fertilization capacity. The aim of this review of recent studies is to select natural ingredients able to reduce oxidative stress. A combination of vitamins (B, C and E), minerals (selenium, iodine) and myo-inositol could be useful as an alternative way, on top of balanced diet and lifestyle advice, for women planning to become pregnant including those with or without SOPK.
Micronutrition and fertility problems in women: What is essential?. Available from: https://www.researchgate.net/publication/319078771_Micronutrition_and_fertility_problems_in_women_What_is_essential?ev=publicSearchHeader&_sg=OLkflgbUBKR-DW8BnuhjARU6gATKsqVmAZziZwYqFsGhEAPbuv8Sktg1NM4DT_khpyLjwXNZ0JcnnAw
The effect of micronutrient supplements on female fertility.
Abstract
Purpose of Review: Benefit of micronutrient supplementation on female fertility.
Recent Findings: Reports of randomized trials are rare. Most studies are focused on multivitamin supplementations. For some micronutrients, a positive impact on fertility could be shown. This article reviews the available clinical studies as well as the pathophysiological background of possible effects and summarizes the potential benefits of selected micronutrients on female fertility.
Summary: Apart from lowering the malformation risk by periconceptional supplementation of folic acid, substitution with different micronutrients, particularly folic acid, vitamin B6, vitamin C, vitamin D, vitamin E, iodine, selenium, iron, and DHA might have a positive impact on infertility treatment. The multivitamin formulation should take the pathophysiology, clinical studies, and upper limits into account.
https://www.ncbi.nlm.nih.gov/pubmed/23571830
Antioxidants for female subfertility.
Showell MG1, Mackenzie-Proctor R, Jordan V, Hart RJ.
Abstract:
Background: A couple may be considered to have fertility problems if they have been trying to conceive for over a year with no success. This may affect up to a quarter of all couples planning a child. It is estimated that for 40% to 50% of couples, subfertility may result from factors affecting women. Antioxidants are thought to reduce the oxidative stress brought on by these conditions. Currently, limited evidence suggests that antioxidants improve fertility, and trials have explored this area with varied results. This review assesses the evidence for the effectiveness of different antioxidants in female subfertility.
Objectives: To determine whether supplementary oral antioxidants compared with placebo, no treatment/standard treatment or another antioxidant improve fertility outcomes for subfertile women.
Search Methods: We searched the following databases (from their inception to September 2016) with no language or date restriction: Cochrane Gynecology and Fertility Group (CGFG) specialized register, the Cochrane Central Register of Studies (CENTRAL CRSO), MEDLINE, Embase, PsycINFO, CINAHL and AMED. We checked reference lists of appropriate studies and searched for ongoing trials in the clinical trials registers.
Selection Criteria: We included randomized controlled trials (RCTs) that compared any type, dose or combination of oral antioxidant supplement with placebo, no treatment or treatment with another antioxidant, among women attending a reproductive clinic. We excluded trials comparing antioxidants with fertility drugs alone and trials that only included fertile women attending a fertility clinic because of male partner infertility.
Data Collection and Analysis: Two review authors independently selected eligible studies, extracted the data and assessed the risk of bias of the included studies. The primary review outcome was live birth; secondary outcomes included clinical pregnancy rates and adverse events. We pooled studies using a fixed-effect model, and calculated odds ratios (ORs) with 95% confidence intervals (CIs) for the dichotomous outcomes of live birth, clinical pregnancy and adverse events. We assessed the overall quality of the evidence by applying GRADE criteria.
Main Results: We included 50 trials involving 6510 women. Investigators compared oral antioxidants, including combinations of antioxidants, N-acetyl-cysteine, melatonin, L-arginine, myo-inositol, D-chiro-inositol, carnitine, selenium, vitamin E, vitamin B complex, vitamin C, vitamin D+calcium, CoQ10, pentoxifylline and omega-3-polyunsaturated fatty acids versus placebo, no treatment/standard treatment or another antioxidant.Very low-quality evidence suggests that antioxidants may be associated with an increased live birth rate compared with placebo or no treatment/standard treatment (OR 2.13, 95% CI 1.45 to 3.12, P > 0.001, 8 RCTs, 651 women, I2 = 47%). This suggests that among subfertile women with an expected live birth rate of 20%, the rate among women using antioxidants would be between 26% and 43%.Very low-quality evidence suggests that antioxidants may be associated with an increased clinical pregnancy rate compared with placebo or no treatment/standard treatment (OR 1.52, 95% CI 1.31 to 1.76, P < 0.001, 26 RCTs, 4271 women, I2 = 66%). This suggests that among subfertile women with an expected clinical pregnancy rate of 22%, the rate among women using antioxidants would be between 27% and 33%. Heterogeneity was moderately high.There was insufficient evidence to determine whether there was a difference between the groups in rates of miscarriage (OR 0.79, 95% CI 0.58 to 1.08, P = 0.14, 18 RCTs, 2834 women, I2 = 23%, very low quality evidence). This suggests that, among subfertile women with an expected miscarriage rate of 7%, use of antioxidants would be expected to result in a miscarriage rate of between 4% and 7%. There was also insufficient evidence to determine whether there was a difference between the groups in rates of multiple pregnancy (OR 1.00, 95% CI 0.73 to 1.38, P = 0.98, 8 RCTs, 2163 women, I2 = 4%, very low quality evidence). This suggests that among subfertile women with an expected multiple pregnancy rate of 8%, use of antioxidants would be expected to result in a multiple pregnancy rate between 6% and 11%. Likewise, there was insufficient evidence to determine whether there was a difference between the groups in rates of gastrointestinal disturbances (OR 1.55, 95% CI 0.47 to 5.10, P = 0.47, 3 RCTs, 343 women, I2 = 0%, very low quality evidence). This suggests that among subfertile women with an expected gastrointestinal disturbance rate of 2%, use of antioxidants would be expected to result in a rate between 1% and 11%. Overall adverse events were reported by 35 trials in the meta-analysis, but there was insufficient evidence to draw any conclusions.Only one trial reported on live birth, clinical pregnancy or adverse effects in the antioxidant versus antioxidant comparison, and no conclusions could be drawn.Very low-quality evidence suggests that pentoxifylline may be associated with an increased clinical pregnancy rate compared with placebo or no treatment (OR 2.07, 95% CI 1.20 to 3.56, P = 0.009, 3 RCTs, 276 women, I2 = 0%). This suggests that among subfertile women with an expected clinical pregnancy rate of 25%, the rate among women using pentoxifylline would be between 28% and 53%.There was insufficient evidence to determine whether there was a difference between the groups in rates of miscarriage (OR 1.34, 95% CI 0.46 to 3.90, P = 0.58, 3 RCTs, 276 women, I2 = 0%) or multiple pregnancy (OR 0.78, 95% CI 0.20 to 3.09, one RCT, 112 women, very low quality evidence). This suggests that among subfertile women with an expected miscarriage rate of 4%, the rate among women using pentoxifylline would be between 2% and 15%. For multiple pregnancy, the data suggest that among subfertile women with an expected multiple pregnancy rate of 9%, the rate among women using pentoxifylline would be between 2% and 23%.The overall quality of evidence was limited by serious risk of bias associated with poor reporting of methods, imprecision and inconsistency.
Authors' Conclusions: In this review, there was very low-quality evidence to show that taking an antioxidant may provide benefit for subfertile women, but insufficient evidence to draw any conclusions about adverse events. At this time, there is limited evidence in support of supplemental oral antioxidants for subfertile women.
https://www.ncbi.nlm.nih.gov/pubmed/28752910
Female dietary antioxidant intake and time to pregnancy among couples treated for unexplained infertility.
Ruder EH1, Hartman TJ2, Reindollar RH3, Goldman MB4.
Abstract:
Objective: To determine whether increased antioxidant intake in women is associated with shorter time to pregnancy (TTP) among a cohort of couples being treated for unexplained infertility.
Design: Secondary data analysis of a randomized controlled trial.
Setting: Academic medical center associated with a private infertility center.
Patients: Females with unexplained infertility.
Interventions: None.
Main Outcome Measure(s): The time it took to establish a pregnancy that led to a live birth.
Result(s): Mean nutrient intake exceeded the estimated average requirement (EAR) for vitamins C and E. No differences in mean intake of any of the antioxidants were noted between women who delivered a live-born infant during the study period vs. those who did not. In multivariable models, intake of β-carotene from dietary supplements was associated with shorter TTP among women with body mass index (BMI) ≥25 kg/m(2) (hazard ratio [HR] 1.29, 95% confidence interval [CI] 1.09-1.53) and women <35 y (HR 1.19, 95% CI 1.01-1.41). Intake of vitamin C from dietary supplements was associated with shorter TTP among women with BMI <25 kg/m(2) (HR 1.09, 95% CI 1.03-1.15) and women <35 y (HR 1.10, 95% CI 1.02-1.18). Intake of vitamin E from dietary supplements among women ≥35 y also was associated with shorter TTP (HR 1.07, 95% CI 1.01-1.13).
Conclusion(s): Shorter TTP was observed among women with BMI <25 kg/m(2) with increasing vitamin C, women with BMI ≥25 kg/m(2) with increasing β-carotene, women <35 y with increasing β-carotene and vitamin C, and women ≥35 y with increasing vitamin E.
CLINICAL TRIAL REGISTRATION NUMBER:
Fertilichron male Research:
Indications of the mechanisms involved in improved sperm parameters by zinc therapy(n=45, controlled trail per 3 month).
Omu AEet al., Med Princ Pract 2008
Abstract:
Objective: To determine possible indications of the mechanisms involved in improved sperm parameters by zinc therapy in asthenozoospermic men.
Subjects and Methods: Forty-five men with asthenozoospermia (>or=40% immotile sperm) were randomized into four therapy groups: zinc only: n = 11; zinc + vitamin E: n = 12 and zinc + vitamins E + C: n = 14 for 3 months, and non-therapy control group: n = 8. Semen analysis was done according to WHO guidelines. Malone dialdehyde, tumour necrosis factor-alpha (TNF-alpha), total antioxidant capacity, superoxide dismutase (SOD) and glutathione peroxidase were determined in the semen and serum. Antisperm antibodies IgG, IgM and IgA were evaluated by immunobeads. Sperm chromatin integrity was determined by acid denaturation by acridine orange and sperm apoptosis by light and electron microscopy. The effect of zinc on in vitro induced sperm oxidative stress by NADH was evaluated.
Results: Asthenozoospermia was significantly associated with oxidative stress with higher seminal malone dialdehyde (8.8 vs. 1.8 mmol/l, p < 0.001) and TNF-alpha (60 vs. 12 pg/l, p < 0.001), and low total antioxidant capacity (1.8 vs. 8.4, p < 0.01), SOD (0.8 vs. 3.1, p < 0.01) and glutathione peroxidase (1.6 vs. 4.2, p < 0.05), compared to normozoospermia. Zinc therapy alone, in combination with vitamin E or with vitamin E + C were associated with comparably improved sperm parameters with less oxidative stress, sperm apoptosis and sperm DNA fragmentation index (DFI). On the whole, there was no difference in the outcome measures between zinc only and zinc with vitamin E and combination of vitamins E + C. In the in vitro experiment zinc supplementation resulted in significantly lower DFI (14-29%, p < 0.05) compared to zinc deficiency.
Conclusion: Zinc therapy reduces asthenozoospermia through several mechanisms such as prevention of oxidative stress, apoptosis and sperm DNA fragmentation.
Effects of xinxibao (Zinc plus Selene) on sperm quality in oligoasthenozoospermic men (n=34, open trail per 3 month).
Shi Yet al., Zhonghua Nan Ke Xue 2004
Abstract:
Objective: To evaluate the effects of zinc and selenium on the sperm quality of oligoasthenozoospermic men.
Methods: Thirty-four cases of oligoasthenozoospermia were treated with Xinxibao (Zinc & Selenium Tablet) three times a day and five tablets at a time for ninety days in succession. The seminal routine analysis was performed by computer-assisted sperm analysis (CASA) at the end of each month.
Results: The sperm quality was improved significantly sixty days and ninety days after treatment. Five cases (14.7%) showed remarkable effect, 25 (73.5%) improved, and 4 (11.8%) did not respond.
Conclusion: Zinc and selenium can significantly improve the sperm quality of oligoasthenozoospermic men.
Relevance of zinc in human sperm flagella and its relation to motility.
Henkel Ret al.,Fertil Steril 1999
Abstract:
Objective: To measure the zinc content of human sperm flagella and to analyze its relation to sperm motility.
Design: Prospective study.
Setting: Center of Dermatology and Andrology.
Patient(s): Semen samples collected from 90 andrology patients and healthy donors after 3-5 days of sexual abstinence.
Intervention(s): None.
Main Outcome Measure(s): Sperm morphology after Shorr staining, sperm motility, and patient age were recorded. In addition, zinc concentrations in the seminal plasma, sperm heads, and flagella were determined with the use of atomic absorption spectrometry.
Result(s): The mean zinc concentration was 144.3 mg/l in the seminal plasma and 146.9 mg/l in the whole ejaculate and was significantly correlated with parameters of motility. The sperm heads contained only 6.7% of the zinc that was present in the whole spermatozoon. The zinc concentration in the flagella was negatively correlated with sperm motility and velocity. In addition, it was positively correlated with the percentage of abnormally blue-stained flagella and the age of the patients.
Conclusion(s): Our results clearly demonstrate the importance of zinc elimination during epididymal sperm maturation for functional competence of the outer dense fibers and, therefore, generation of motility.
https://www.ncbi.nlm.nih.gov/pubmed/10360924
Human sperm chromatin stabilization: a proposed model including zinc bridges.
(review).
Bjorndahl L; Kvist U
Mol Hum Reprod 2010 Jan
Abstract: The primary focus of this review is to challenge the current concepts on sperm chromatin stability. The observations (i) that zinc depletion at ejaculation allows a rapid and total sperm chromatin decondensation without the addition of exogenous disulfide cleaving agents and (ii) that the human sperm chromatin contains one zinc for every protamine for every turn of the DNA helix suggest an alternative model for sperm chromatin structure may be plausible. An alternative model is therefore proposed, that the human spermatozoon could at ejaculation have a rapidly reversible zinc dependent chromatin stability: Zn(2+) stabilizes the structure and prevents the formation of excess disulfide bridges by a single mechanism, the formation of zinc bridges with protamine thiols of cysteine and potentially imidazole groups of histidine. Extraction of zinc enables two biologically totally different outcomes: immediate decondensation if chromatin fibers are concomitantly induced to repel (e.g. by phosphorylation in the ooplasm); otherwise freed thiols become committed into disulfide bridges creating a super stabilized chromatin. Spermatozoa in the zinc rich prostatic fluid (normally the first expelled ejaculate fraction) represent the physiological situation. Extraction of chromatin zinc can be accomplished by the seminal vesicular fluid. Collection of the ejaculate in one single container causes abnormal contact between spermatozoa and seminal vesicular fluid affecting the sperm chromatin stability. There are men in infertile couples with low content of sperm chromatin zinc due to loss of zinc during ejaculation and liquefaction. Tests for sperm DNA integrity may give false negative results due to decreased access for the assay to the DNA in super stabilized chromatin.
Does folic acid and zinc sulphate intervention affect endocrine parameters and sperm characteristics in men?
(n=47 fertile, 40 subfertile, double blind, placebo controlled trail per 26 weeks).
Ebisch IMet al., Int J Androl 2006
Abstract: We evaluated pre- and post-intervention endocrine and semen parameters in a double-blind, placebo-controlled intervention study to investigate the underlying mechanism of increased sperm concentration after folic acid and zinc sulphate intervention. A total of 47 fertile and 40 subfertile males participated in a 26-week intervention study consisting of a daily treatment with folic acid (5 mg/day) and zinc sulphate (66 mg/day), or placebo. Pre- and post-intervention semen parameters, serum folate, zinc, follicle-stimulating hormone (FSH), testosterone and inhibin B concentrations were measured. The results indicated that intervention treatment significantly increased sperm concentration in subfertile males. Other semen and endocrine parameters were not affected by intervention treatment. At baseline, positive correlations were found between serum zinc and sperm concentration, motility and inhibin B. Serum zinc and FSH were inversely correlated. As (already) well known from previous research, inhibin B positively correlated with sperm concentration, motility and morphology, and was inversely correlated with FSH. The latter was positively correlated with testosterone. In addition, testosterone and inhibin B were inversely correlated. After intervention, the correlations with zinc disappeared. We conclude that the increase in sperm concentration after folic acid and zinc sulphate intervention is not the result of alterations in FSH, testosterone or inhibin B concentrations. Although zinc and folate have several effects on spermatogenesis, the underlying mechanisms involved are not clear.
One-carbon cycle support rescues sperm damage in experimentally induced varicocoele in rats.
Mohammadi P1,2, Hassani-Bafrani H2,3, Tavalaee M1, Dattilo M4, Nasr-Esfahani MH1,5.
Abstract:
Objectives: To investigate whether micronutrients in support of the one-carbon cycle and glutathione synthesis are effective in improving sperm damage after surgical varicocele induction in rats and whether any effect is achieved without a rebound reductive stress as seen with oral antioxidants.
Materials and Methods: Surgical varicocele was induced in adult male Wistar rats and resulted in significant damage to the testis and sperm cells measured at 2 and 4 months after surgery. At 2 months after surgery, rats received a 2-month oral supplementation in support of the one-carbon cycle containing B vitamins (B2, B3, B6, folic acid and B12), N-acetyl-cysteine, zinc, small amounts of vitamin E, and a natural source of betalains and quercetine (Condensyl® ; Parthenogen SAGL, Lugano, Switzerland and Nurilia SARL, Lyon, France).
Results: One-carbon cycle supplementation, compared to untreated controls, significantly improved the morphometric characteristics of testis (P < 0.05), sperm concentration, motility and abnormal morphology (P < 0.001), sperm chromatin condensation (aniline blue staining, P < 0.05), sperm DNA damage (acridine orange staining, P < 0.05) and sperm lipid peroxidation (BODIPY C11, P < 0.001). The improvement in both nuclear condensation and DNA damage and the lack of excessive inhibition of lipid peroxidation confirmed that no reductive stress had occurred.
Conclusions: Micronutrients in support of the one-carbon cycle are effective in the treatment of surgically induced varicocoele in rats, probably by activating natural antioxidant defences and epigenetics. These results support the idea that essential micronutrients including B vitamins may also have a positive influence in clinical varicocoele, which should be tested in prospective clinical trials.
https://www.ncbi.nlm.nih.gov/pubmed/29752770
Lipovac M, Bodner F, Imhof M, Chedraui P.
Reprod Biol Endocrinol.2016 Dec 9;14(1):84.
Comparison of the effect of a combination of eight micronutrients versus a standard mono preparation on sperm parameters.
Abstract:
Background: There are reports showing that l-carnitine alone or in combination with other micronutrients improve sperm parameters. However, comparative studies are still lacking. This study was carried out to compare the short term effects of a combination of eight micronutrients including l-carnitine vs. a mono-substance (l-carnitine alone) on sperm parameters.
Methods: This was a prospective, open-labelled, nonrandomized study that included male subjects (20 to 60 years) with at least 1 year of subfertility and at least one pathological semen analysis who received 3 months treatment with a mono-substance (500 mg l-carnitine/twice a day, n = 156) or a combined compound (440 mg l-carnitine + 250 mg l-arginine + 40 mg zinc + 120 mg vitamin E + 80 mg glutathione + 60 μg selenium + 15 mg coenzyme Q10 + 800 μg folic acid/once a day, n = 143) for the same time period. Sperm parameters were analyzed before and after treatment and groups comparisons performed.
Results: Baseline characteristics were similar among studied groups (age and body mass indices). Semen parameters (volume, density, overall progressive motility [including slow and fast motility]) and percentage of sperm with normal morphology improved after 3 months in both groups as compared to baseline. However, relative change (expressed as % increase of absolute values) for sperm density and overall progressive motility (including fast motility) was found to be higher for the combined micronutrient treatment group as compared to the mono-treatment using l-carnitine alone.
Conclusion: Both analyzed groups displayed a positive short term effect on all sperm parameters; however effect on density and motility was significantly better for the combined formulation. There is need for more research in this matter that includes long term outcome data.
Azizollahi G, Azizollahi S, Babaei H, Kianinejad M, Baneshi MR, Nematollahi-mahani SN.
J Assist Reprod Genet.2013 Apr;30(4):593-9. doi: 10.1007/s10815-013-9961-9. Epub 2013 Feb 24.
Effects of supplement therapy on sperm parameters, protamine content and acrosomal integrity of varicocelectomized subjects.
Abstract:
Purpose: Surgical repair of varicocele has long been a procedure to correct spermatogenesis. However, the outcome has been reported to be inadequate. We combined varicocelectomy with supplement therapy to evaluate the concurrent effect of these procedures.
Methods: A prospective randomized controlled study was undertaken to investigate the effects of zinc sulfate, folic acid and zinc sulfate/folic acid on sperm quality, protamine content and acrosomal integrity following surgical repair of varicocele. Male subjects with palpable varicocele were included in the study and randomized into four groups. Subjects received Zinc sulfate, Folic acid, Zinc sulfate/Folic acid or placebo for 6 months. A semen sample was obtained before surgery and 3 and 6 months after surgical repair. Semen samples were evaluated for sperm parameters as well as chromatin content and acrosomal integrity.
Results: Most of the evaluated parameters showed a mild improvement after varicocelectomy in the placebo group. Interestingly, co-administration of Zinc sulfate and folic acid improved most factors significantly. Folic acid administration but not zinc sulfate could increase sperm number. Hence, Zinc sulfate was better than folic acid when change in morphology was assessed, and none of them was significantly effective in sperm motility. In Zinc sulfate and Folic acid groups, protamine content and halo formation rate significantly improved.
Conclusions: We may conclude that co-administration of zinc and folic acid significantly improved sperm parameters and increased varicocelectomy outcomes. So, medical treatment with compatible drugs after surgery might be advantageous for obtaining acceptable results.
Fertilichron female Research:
Zinc availability regulates exit from meiosis in maturing mammalian oocytes
Nature Chemical Biology volume6, pages674–681 (2010) | Download Citation
Abstract: Cellular metal ion fluxes are known in alkali and alkaline earth metals but are not well documented in transition metals. Here we describe major changes in the zinc physiology of the mammalian oocyte as it matures and initiates embryonic development. Single-cell elemental analysis of mouse oocytes by synchrotron-based X-ray fluorescence microscopy (XFM) revealed a 50% increase in total zinc content within the 12–14-h period of meiotic maturation. Perturbation of zinc homeostasis with a cell-permeable small-molecule chelator blocked meiotic progression past telophase I. Zinc supplementation rescued this phenotype when administered before this meiotic block. However, after telophase arrest, zinc triggered parthenogenesis, suggesting that exit from this meiotic step is tightly regulated by the availability of a zinc-dependent signal. These results implicate the zinc bolus acquired during meiotic maturation as an important part of the maternal legacy to the embryo.
https://www.nature.com/articles/nchembio.419?page=2
Assessment of dietary intake and mineral status in pregnant women.
Kocyłowski R1,2, Lewicka I3, Grzesiak M4, Gaj Z1,5, Sobańska A3, Poznaniak J3, von Kaisenberg C6, Suliburska J7.
Abstract:
Purpose: To evaluate the dietary intake of pregnant women and their nutritional status of Ca, Mg, Fe, Zn, and Cu, as the nutritional status of pregnant women is an important factor for the proper progression of a pregnancy and the development and health of the fetus.
Methods: The study was conducted on 108 pregnant women ages 18-42, at 6-32 weeks of gestation. We used a questionnaire and a 24-h recall nutrition interview. Hair samples were taken for testing and the level of each mineral was assessed using atomic absorption spectrometry. The results were analysed using the Dietetyk and Statistica 10 software.
Results: Low levels of Fe, Zn, Ca, Mg, vitamin D, and folic acid intake were seen in the pregnant women, with the use of dietary supplements significantly increasing their intake of Fe, Zn, and folic acid. The concentration of zinc and magnesium in the women's hair was shown to be affected by their age and, in the case of magnesium, by the week of pregnancy.
Conclusions: It was observed that the diet of pregnant women is characterized by low levels of Fe, Zn, Ca, Mg, vitamin D, and folic acid. Dietary supplementation with vitamins and minerals significantly increases the daily Fe and folic acid intake in pregnant women. The concentration of Zn and Mg in hair depends on the age of pregnant women and Mg level in the hair of women decreases during pregnancy.

